Sleep disorders and Central Sleep Apnea Syndrome, CSAS
Chapters on this page
-
Healthy sleep and sleep stages
-
Sleep affects the following matters:
-
-
Influence of Light on Sleep / Biological Clock WINTER TIME SUMMER TIME Tips
-
-
Sleep disorders due to brain injury
-
-
Multiple sleep disorders examined (including OSAS sleep apnea)
-
CSAS, Central Sleep Apnea Syndrome
-
Hypoventilation and hypercapnia
-
Treatment of CSAS and hypercapnia
Healthy sleep
Healthy sleep is a certain degree of unconsciousness. It is regulated by the biological clock, also called the day-night rhythm, biorhythm or circadian rhythm. This rhythm is regulated by the hypothalamus. The biological clock responds to light stimuli and when it gets darker it starts producing the sleep hormone melatonin in the pineal gland (epiphysis).
The biorhythm is partly hereditary.
A normal sleep cycle has four sleep stages. Each sleep cycle lasts about 90-120 minutes. In a good night, a person can go through four to five of these sleep cycles.
Stage 1 and 2
Light sleep, the transition from being awake to falling asleep. Breathing becomes slower, heart rate becomes a bit slower and body temperature drops a bit. Muscles relax and sometimes contract a bit, the well-known jerk or sleep spasm. You wake up in this stage from sounds. This stage is also called Slow Eye Movements sleep (SEM). Characteristic is that the eyes slowly roll away when you fall asleep.
Stage 2
This stage is sometimes called a deeper sleep stage and lasts about 30 to 40 minutes. It is the beginning of real sleep.
Phase 3
This phase is Delta sleep. On an EEG (Electroencephalogram or brain film) you can observe the typical slow delta waves (slow wave sleep). The Delta sleep is the very deep sleep.
In this sleep phase, growth hormone is produced and this allows our body to recover: it is good for the bones and there is recovery of muscle tissue. At the beginning of the night, this phase lasts the longest and in the subsequent cycles it is shorter.
Phase 4
This phase is REM sleep. REM stands for Rapid Eye Movement. Typical for this sleep phase is that during a dream the eyes move back and forth. In this phase, the large muscles of the limbs, from the neck (pons) downwards, are in a state of relaxation. They become slack as in a 'paralysis'. As a result, the dreams cannot be carried out by the body, as sometimes happens with abnormal REM sleep behaviour. As the night progresses, the periods of REM sleep become longer.
As a person gets older, the deep sleep phases can become shorter and people then feel less rested when they wake up.
When someone sleeps well, that person spends 20 to 25% of their time in REM sleep. The other phases are called Non-REM sleep: NREM. In Non-REM sleep, the muscles are still mobile and there is not much activity in the brain.
One sleep cycle of 90-120 minutes

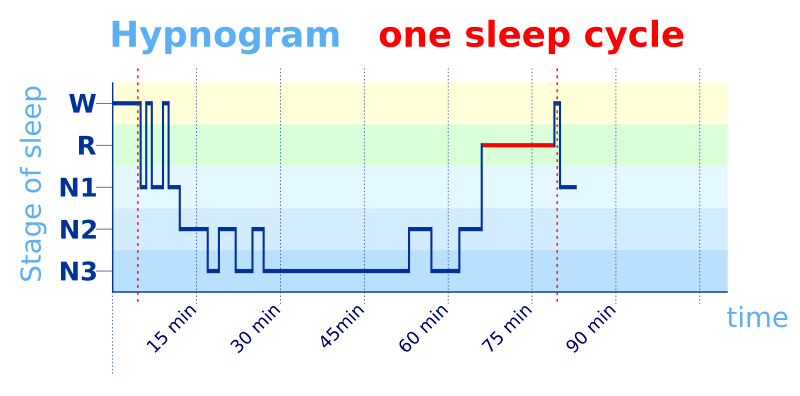
W: awake (yellow) R: Rem sleep (green) N1,N2,N3: Non Rem sleep (blue)
Image on the left: public domain By gif: en.user svg: Krzysztof Szymański (Krzysiu Jarzyna) - From en.wikipedia (permition granted by the creator, inthe English Wikipedia),Public Domain,
https://commons.wikimedia.org/w/index.php?curid=1708491
Image on the right: By Schlafgut - Own work, CC BY-SA 3.0,
https://commons.wikimedia.org/w/index.php?curid=24139956
Sleep affects the following matters
-
health
-
disease
-
performance, thinking, skills, alertness, road safety
-
emotions and emotion regulation
Health
Especially during deep sleep, the brain cells are ‘washed clean’. During the day, every person produces ‘toxic’ waste products, which must be removed to the lymphatic system.
Certain cells are very important in this: the glial cells.
Previously, it was thought that they were only supporting cells and filled the spaces between the brain cells.
We now know that during sleep, the glial cells slowly become smaller, causing the space around them, which is filled with fluid, to become larger.
The glial cells have hydrogen channels and the process of becoming smaller triggers a fluid system. This cleans the brain cells.
Sleep is also important for the immune system. Sleep ensures that more antibodies are produced that play a role in attacking pathogens. Sleep also makes the memory of the immune system stronger.
Chronic sleep deprivation and disease
Population studies have shown that chronic sleep deprivation is linked to heart disease, type 2 diabetes, cancer, weight gain, obesity, depression, anxiety, mood disorders and more.
Risk factor for Alzheimer's
A sleep disorder is not only a risk factor for the development of a number of mental disorders, but it can even increase the chance of getting Alzheimer's disease.
That is, if there is a chronic and very long-term lack of sleep.
The small waste products that are flushed out during sleep are the same toxins that go wrong in Alzheimer's disease.
Alarm signal for a serious condition
A sleep disorder can also be an alarm signal for a serious psychological or physical (somatic) condition. Sleep complaints can be a sign of the presence of neurological and other somatic problems such as heart failure, osteoarthritis and Parkinson's disease.
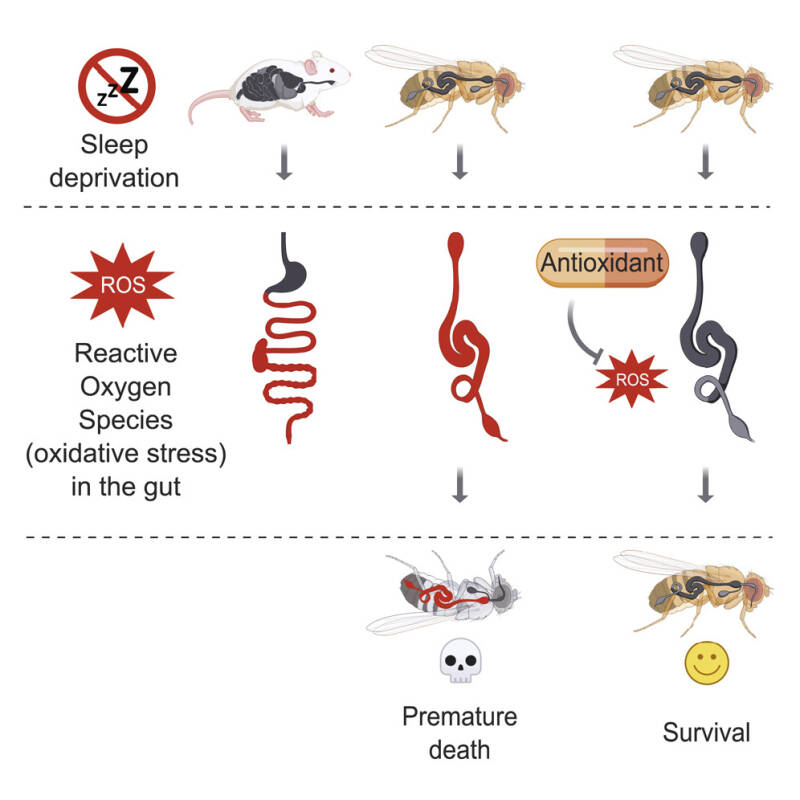
Damage to the intestines with accumulation of harmful oxidants, premature death?
A sleep disorder even causes damage to the intestines.
This was shown by a study by Harvard University in 2020 in which fruit flies (Drosophila) were studied.
Fruit flies have surprisingly many similarities with human genes. Where a fruit fly normally lives for forty days, they died after ten to twenty days if they were kept awake. Microscopic examination showed that there was a lot of damage in the intestines of the fruit flies in particular. Harmful oxidants accumulated there, causing premature death. But if the flies were given antioxidants, they survived the full forty days, despite the lack of sleep. This could be important for the future to promote health.
See image from marlin-prod.literatumonline
Performance, thinking ability, making crucial mistakes, traffic safety and overestimating yourself
Sleep also has a huge influence on thinking and the ability to perform tasks. Think of traffic safety.
Someone who is awake for more than seventeen hours performs just as poorly on tasks as someone who has had two glasses of an alcoholic drink. When a person is tired, he or she can no longer make crucial decisions.
In a fourteen-day study, people who were deprived of sleep made a lot of mistakes. After three days, the study stopped for them.
The people who got four hours of sleep a night also made a lot of mistakes over a longer period of time and were at the same level as the first group without sleep.
The group that got six hours of sleep a night initially performed better, but even after those fourteen days it turned out that they had also ended up in the danger zone for making crucial mistakes, just as much as those who had not slept at all for a whole night.
However, it was striking that this group did not actually feel tired or sleepy and the people reported that they did feel good. The objective assessment and estimation of one's own performance was gone! After all, these people all made crucial mistakes. Overestimating one's own ability to perform after sleep deprivation can have enormous consequences for example on driving skills or having to deliver top performances, both physically and in thinking.
Overestimating your own performance after sleep deprivation can have huge consequences on, among other things, your driving skills. This can lead to very serious accidents.

Emotions and emotion regulation
More intense emotions and less effective emotional decisions
When a person has not slept, er or his emotions can become more intense. The emotional decisions can be less effective or this person cannot regulate the emotions.
The cerebral cortex of the frontal lobe, where the thinking capacity, the ratio is located, may function less well due to little sleep and may therefore inhibit the emotions less well.
The center of the emotions is located in both amygdala's (in the left and right hemispheres). The frontal lobe (particularly the medial prefrontal cortex) normally inhibits the amygdala.
Anxiety and mood disorders
There is evidence that there is a close and causal relationship between sleep and emotional mood (affective brain regulation). See for example here.
Almost all mood and anxiety disorders occur together with one or more sleep disorders.
The amygdala also plays a role here. Lack of sleep is related to the increased sensitivity (sensitization) of the amygdala, which causes an increased fear response.
A lack of sleep therefore disrupts the processing of fear in the brain. Poor sleep makes people more susceptible to anxiety disorders. During sleep, a person is optimally prepared for social and emotional functioning the next day.
Closeness and Loneliness
A lack of sleep can reduce the ability to feel close to others and can affect relationships.
A study found that after a good night's sleep, people let others get fairly close, but after a bad night's sleep, people kept others at a greater distance. This can have serious consequences for loneliness over time.
Sleep needs by age
| Age and condition | Average hours of sleep per 24 hours |
|---|---|
| newborn | up to 18 hours |
| 1 to 12 months | 14 - 18 hours |
| 1 to 3 years | 12 - 15 hours |
| 3 to 5 years | 11 - 13 hours |
| 5 to 12 years | 9 - 10 hours |
| older teens / adolescents | 8 - 10 hours |
| adults and elderly | 7 - 8 hours |
| pregnant women | 8 (+) hours |
Influence of light on sleep / biological clock
Did you know that seeing light influences your biological clock?
A small group of nerve cells regulates sleep through the incidence of light. These nerve cells are located together in the suprachisamatic nucleus (SCN) or 'nucleus suprachiasmaticus', which, as the name suggests, is located just above the chiasma opticum.
That is where the optic nerves cross. So close to the eyes, which bring the light to this nucleus via light-sensitive cells in the retina.
So the biological clock is literally in your head and is no bigger than the period after this sentence.
The biological clock triggers the pineal gland to produce more or less melatonin (sleep hormone).
At normal light intensity, LED light or screen light (the so-called blue light), less melatonin is released via this brain nucleus and sleep is inhibited.
Exposure to bright light late in the evening therefore disrupts the ability to fall asleep properly.
Conversely, a completely darkened room prevents you from waking up properly in the morning.
The biological clock also influences body temperature. It is slightly higher in the evening and drops during the night. It is lowest in the morning. If you are too warm, you cannot sleep well. But if you have cold feet, you cannot fall asleep. Digestion also slows down at night.
Our sleep-wake rhythm is therefore accompanied by a day-night rhythm / biological clock.
Different time zones and night shifts
Anyone who has ever traveled knows that jet lag can occur because you live in a different time zone.
Jet lag is a disruption of the sleep-wake rhythm.
People who have to work during the night also experience such a disruption of the biological clock. This is the case the first night(s)
and also when they have to switch back to daytime life.
Tips for switching to winter time
Because your biological clock, your sleep-wake rhythm, is influenced by light, you can play with it a bit.
You shift the biological clock very gently if you take in a bit more light in the evening and don't turn on the lights or look at your screen in the morning. If you don't open the curtains right away, but keep it a bit dim for an hour, the biological clock gets used to it and shifts to a later time.
A week in advance, eat a quarter of an hour later every day and go to bed a bit later. Go to bed an hour later the night before winter time starts, so that you wake up on Sunday at your 'normal' time.
To switch to wintertime, the clock goes backward an hour. The clock goes from 3 a.m. to 2 a.m.
In the winter, we are more in our natural rhythm.
Tips for switching to summer time (daylight saving time)
Get used to having your meals a little earlier until eventually an hour earlier.
Avoid blue light (screens) and LED lights.
In the morning, open the curtains immediately and look into the light! To switch to summertime, in spring, the clock goes forward an hour. The clock goes from 2 a.m. to 3 a.m.
People with brain injuries have a little more difficulty switching to summer time because we are more in our natural rhythm in the winter.
When should you consult a specialist for sleep problems?
It is advisable to be referred to a sleep specialist:
- In case of severe daytime sleepiness.
- In case of risk factors for sleep apnea (e.g. daytime sleepiness, headaches when getting up (and history of brain injury) or snoring and obesity)
- In case of unusual or dangerous behavior during sleep (e.g. REM sleep behavior disorder)
- In cases of insomnia associated with non-response to usual behavioral approaches or medication
- In case of atypical symptoms or for refractoriness to treatment
Sleep disorder due to brain injury
A sleep disorder as a result of Acquired Brain Injury appears to occur more often than was previously thought. Sleep is necessary to maintain concentration and thinking ability. Sleep is also necessary for health, see the paragraph earlier on this page.
Topics covered in this section:
- sleeping too much and the risks of this
- not being able to fall asleep
- waking up too often and not being able to sleep through the night
- sleeping too little, waking up too early
- breathing stops (apnea due to obstruction in the throat or because the brain does not control the lungs sufficiently)
- intense fatigue and heavy head during the day/morning
too much carbon dioxide (hypercapnia) - grinding of teeth
- intense dreaming and sleepwalking
- making wild movements during sleep
- cramps in the legs
Be alert for injuries in brain areas
The following brain areas should be checked for abnormalities:
Diaphragm weakness or paralysis (diaphragm dysfunction or diaphragmatic paresis). Is the diaphragm sufficiently controlled by the brain? This can be measured with an outpatient night registration.
Are there multiple respiratory arrests during the night during a registration?
Does the person wake up with a headache? Is he or she too tired to get through the day?
We only speak of a sleep disorder if a person has had poor sleep for more than a month and is bothered by this during the day.
Proper treatment of sleep disorders caused by brain injury usually leads to improvement of cognitive and psychological problems and improvement of energy and work performance. A well-treated sleep disorder can also reduce headaches and existing depression and prevent serious physical complications. According to a study, sleeping too much or too little can affect memory.
In which brain disorders?
Traumatic brain injury: 40-65% of people with traumatic brain injury complain of insomnia. Studies show that sleep disorders occur three times more often in people with traumatic brain injury than in healthy people. People with a stroke/cerebral hemorrhage or infarction can also have sleep problems.
Stroke/CVA: It is estimated that 60% of people with a stroke have a sleep disorder.
People with a brainstem infarction or a brainstem hemorrhage are particularly known to develop sleep disorders.
Conversely, sleep apnea (breathing arrest during sleep) can also cause a cerebral infarction!
Neurodegenerative diseases
Characteristic of neurodegenerative diseases such as Parkinson's disease and multi-system atrophy (MSA) are sleep disorders. These are mainly the REM sleep related disorders.
A REM sleep behavior disorder is also a predictor of neurodegenerative diseases.
In 70 to 80% of people who have a REM sleep behavior disorder, a neurodegenerative disorder (alpha-synuclein disorder) develops within a period of about ten to twelve years.
REM sleep disorder with wild movements
REM sleep is the dream sleep. It is named after Rapid Eye Movement, because the eyes move back and forth during a dream sleep. The other muscles are completely slack.
Someone with a REM sleep-related disorder (REM sleep behavior disorder) can dream very intensely and even go sleepwalking, because in contrast to a normal REM sleep, the movement muscles are not slack. The dreams are lived out / portrayed with unusually many and often wild movements and making sounds such as shouting and talking. Talking in the sleep is called sleep-talking or somniloguy.
Often a person with a REM sleep behavior disorder has injuries that he or she has inflicted on himself or herself during the wild movements in sleep. A bed partner can also be pushed out of bed or be injured during the dream of the person with this sleep disorder.
Sleep medication may mask problems
Many people with NAH do receive sleep medication to help them fall asleep, but are not set on a normal sleep-wake rhythm. Sleep medication can even worsen an undiscovered and untreated sleep disorder such as CSAS, with potentially (life-)threatening consequences.
We therefore advocate for proper diagnosis if a person with brain damage continues to complain about sleep problems.
Sleeping too much
There have been studies that noted that performance deteriorates with shorter sleep, as we mentioned in the chapter on performance, thinking, skills, alertness, traffic safety.
Other studies have also shown memory impairment and reduced cognitive function in people who sleep too much.
People who slept more than nine hours were 21% more likely to be obese than normal sleepers, according to Canadian researchers
Chaput et al.
A Chinese study links too much sleep to a higher risk of heart attacks and stroke, with a risk of stroke or heart failure increasing by up to 41 percent!
A daytime nap is associated with an increased risk of serious cardiovascular disease (CVD) and death in people who slept more than 6 hours a night, but not in people who slept less than 6 hours a night.
We will continue to look for new studies to keep you informed.
Multiple sleep disorders
In general, sleep disorders are classified into:
1) parasomnias
2) dyssomnias.
We will go into more detail about different specific sleep disorders.
1) Parasomnias are related to abnormal phenomena or behaviors during sleep.
- Excessive movement during sleep, such as sleepwalking (somnabulism)
- Night terrors (pavor nocturnus)
- Sleep drunkenness (RBD = REM Behavior Disorder) which is also seen in MSA, Parkinson's disease and Lewy body dementia
- Teeth grinding (bruxism) can also occur in Parkinson's and Huntington's disease
- Talking in sleep (somniloguy)
2) Dyssomnias are related to the duration, quality and timing of sleep.
- Sleep-wake disorders, including narcolepsy with
daytime sleep attacks that cannot be resisted. Abrupt
muscle relaxation attacks can also occur. - Restless legs syndrome RLS: restlessness or cramps or short-term jerks in the legs - even without the person being aware of it. RLS often occurs together with PLMD
- PLMD: Periodic Limb Movement Disorder. With this sleep disorder
the legs suddenly make violent, jerking movements while during sleep. This happens several times a night. The arms may also make sudden bending and stretching movements during sleep. - Insomnia: problems falling asleep, waking up too early
and then not being able to fall asleep again, waking up often. - Circadian rhythm sleep disorders or CRSD: problems with sleep-wake rhythm and the time at which one can fall asleep. For example, the "delayed sleep phase syndrome".
- Apnea syndrome: Sleep apnea is a cessation of breathing during sleep. If a person has respiratory arrest during sleep more than 5 times per hour, lasting at least 10 seconds, this is called an apnea syndrome.
An apnea can affect the entire body, because the organs do not receive enough oxygen. In addition, someone can remain extremely tired because the body has not been able to recover during the night.
There are two types of sleep apnea. OSAS or CSAS.
These two types of sleep apnea have different causes.
When most people think of sleep apnea, they immediately think of snorers. But not everyone knows that brain damage can cause a form of sleep apnea in which the brain does not sufficiently control the lungs. We describe both forms.- OSAS: Obstructive Sleep Apnea Syndrome. As the name suggests, there is an obstruction. This is because the tongue and soft parts in the throat block breathing. During sleep, the tongue can drop into the throat due to a weak larynx or a too weak trachea. This causes people to snore loudly. An OSAS apnea due to obstruction in the throat can even lead to a risk of a stroke!
In addition to the advice to lose weight if you are overweight, there are two most commonly used treatments for an obstructive sleep apnea syndrome (OSAS): the 'bit/denture' or also called mandibular repositioning device (MRA) and Continuous Positive Airway Pressure therapy (CPAP). The CPAP is a device that provides slight overpressure, which keeps the airways open at night. This can be done via an air hose to a nose mask or nose-mouth mask.
Research shows that a CPAP treatment can improve cognitive functioning in OSAS patients who have had a stroke. - CSAS: Central Sleep Apnea Syndrome. Central means from the brain. The brain does not give enough signal to breathe during sleep.
CSAS is discussed in detail below. Someone with this form of apnea does not necessarily snore.
- OSAS: Obstructive Sleep Apnea Syndrome. As the name suggests, there is an obstruction. This is because the tongue and soft parts in the throat block breathing. During sleep, the tongue can drop into the throat due to a weak larynx or a too weak trachea. This causes people to snore loudly. An OSAS apnea due to obstruction in the throat can even lead to a risk of a stroke!
Central Sleep Apnea Syndrome, CSAS
If the brain does not provide enough stimuli to breathe, this is called central sleep apnea syndrome (CSAS).
The respiratory center in the brain (medulla oblongata in the brainstem) regulates the number of times you breathe and how deeply you breathe. Normally, the brain responds to an increase in carbon dioxide and a decrease in oxygen, after which the signal is sent to the respiratory muscles to breathe.
This can be disrupted in people with brain damage. Particularly in people who have brainstem damage.
People who had a lack of oxygen as the cause of the brain damage are also vulnerable to this condition.
Also patients with multi-system atrophy (MSA) and Parkinson's disease can have this (unnoticed).
Characteristic for this syndrome is the very great difficulty in falling asleep, which can last for hours. The person wakes up several times from a survival reflex because there is no breathing. If this happens very often per night, the person is extremely tired by the time of getting out of bed.
In CSAS, the person is not necessarily snoring during sleep, which does happen in people with Obstructive Sleep Apnea Syndrome (OSAS). Breathing can slow down to 2 to 3 times per minute while 12 to 16 times is normal and can also stop completely.
CSAS occurs in combination with OSAS, Obstructive Sleep Apnea Syndrome, but also occurs alone.
OSAS or CSAS?
OSAS, Obstructive Sleep Apnea Syndrome, may occur because the muscles relax during sleep, causing the tongue and soft parts in the throat to block breathing. Usually loud snoring occurs.
CSAS, Central Sleep Apnea Syndrome is caused by insufficient control of breathing by the brain during sleep. This can be caused by brain damage.
The medulla oblongata is the primary respiratory control center. Its main function is to send signals to the muscles that control breathing to make breathing happen.
In some cases, sleep apnea can even cause a stroke.
Read more about chances.
Click here for more information about OSAS.
Complaints of people with CSAS:
- Sleep problems with frequent waking, restless sleep and not getting into deep sleep
- Difficulty falling asleep
- Drowsiness or severe fatigue during the day
- Often headaches upon waking
- Not feeling rested upon waking
- Often urge to urinate at night
- Insufficient breathing (hypoventilation) and therefore possibly hypercapnia (too much carbon dioxide, especially at night, can be normal during the day)
- Physical complaints in the long term that often seemed inexplicable before
Hypoventilation and hypercapnia
Hypoventilation is the opposite of hyperventilation. There is insufficient effective breathing. With hyperventilation there is too fast breathing and too low carbon dioxide (hypocapnia) and with hypoventilation the opposite: too slow or stopped breathing and too high carbon dioxide (hypercapnia).
Too much carbon dioxide / hypercapnia
Normally, a rising carbon dioxide / carbon dioxide level leads to a breathing stimulus.
Try staying under water in a swimming pool, the stimulus that makes you want to come up for air is the stimulus that makes you gasp for oxygen as a reflex and you start breathing faster.
In people with brain damage, that stimulus to breathe from the brain can disappear during sleep (Central sleep apnea syndrome / CSAS). The brain of people with brain damage gradually become accustomed to the high carbon dioxide / carbon dioxide level.
This leads to acidification of the blood and drowsiness.
Causes of hypercapnia
- Sleep apnea
- Genetic causes
- Nervous and muscle diseases such as ALS (amyotrophic lateral sclerosis), myasthenia gravis, Guillain-Barré syndrome
- Brain inflammation / encephalitis
- Brainstem stroke
- Overdose of opiates or sleeping pills (benzodiazepines)
- Hypothermia of the body
- COPD: hypercapnia can be seen as a complication of COPD. Due to the inability to exhale properly, and therefore air actually remains in the lungs, less carbon dioxide, CO2, can be exhaled.
Carbon dioxide is a waste product of breathing and can cause problems if it cannot be removed sufficiently. Sleep medication can even increase carbon dioxide accumulation or hypercapnia. That is why a good diagnosis is very important.
Danger of hypercapnia
Hypercapnia leads or may lead to
- headache
- increase in blood pressure
- palpitations
- muscle tremors, (tremor and myoclonus)
- confusion
- apathy, drowsiness
- seizures
- loss of consciousness
- coma or death
In brain injury patients with hypercapnia there may be reduced motor skills, depression and memory disorders and nerve pain. There may also be areas of numbness on the skin or itchy areas as if ants were crawling on the skin (neuropathy with paresthesia).
Treatment of CSAS and hypercapnia
Treatment of hypercapnia depends on the severity of the condition, but also on the underlying cause.
If a diagnosis of Central Sleep Apnea / CSAS with nocturnal respiratory arrest and increased carbon dioxide (hypercapnia) is made, the patient can be put on medication or put on BiPAP or Bilevel / Biphase machine.
In this, breathing is done through a nasal mask with the mouth closed and both the inhalation and exhalation are regulated. If the patient is well adjusted, he or she can learn to use the machine and can then be ventilated at home during the night. Sometimes other treatment is considered.
BiPAP: ‘Bi’ stands for Bi-level, because you are helped at two levels when breathing in and out. ‘PAP’ stands for Positive Airway Pressure. This means that there is always a positive pressure in the airways, which allows the air to flow better through the airways and the lungs to get enough fresh air.
Diagnosing CSAS with hypercapnia can only be done in a hospital.
The general practitioner can refer to a lung specialist. The lung specialist will refer to a center for Home Artificial respiration.
A research can be done at home, a sleep registration often with a TOSCA measurement.
A TOSCA measurement uses a sensor that is placed overnight on the forehead and measures the carbonic acid gases through the skin (transcutaneous).
On the basis of these measurements at home it is decided to take a patient to a center for home artificial respiration.
If a diagnosis Central Sleep Apnea / CSAS with nocturnal respiratory arrest, and increase in carbon dioxide (hypercapnia) is made, the patient is adjusted to a BiPAP machine.
By means of this machine the breathing occurs by a nose cap which regulates both the inhalation and the exhalation. When the patient is properly adjusted to the machine he or she can learn to use the machine and can then be ventilated at home during the night.
A BiPAP machine

Resources
Afonso D.J., Liu D., Machado D.R., Pan H., Jepson J.E., Rogulja D., Koh K.
TARANIS Functions with Cyclin A and Cdk1 in a Novel Arousal Center to Control Sleep in Drosophila.
Curr. Biol. 2015; 25: 1717-1726 https://pubmed.ncbi.nlm.nih.gov/26096977/
Alzoubi K.H , Khabour O.F, Salah H.A., Rashid B.A, Damaj I.M, Salah H.A., (2012)
The neuroprotective effect of vitamin E on chronic sleep deprivation-induced memory impairment: the role of oxidative stress. Behav. Brain Res.2012; 226: 205-210 https://pubmed.ncbi.nlm.nih.gov/21944940/
Backgrounder: Later School Start Times. National Sleep Foundation (Undated). "Teens are among those least likely to get enough sleep; while theyneed on average 9 1/4 hours of sleep per night..." https://www.sleepfoundation.org/articles/backgrounder-later-school-start-times
Centrum Thuisbeademing http://www.umcutrecht.nl/nl/Ziekenhuis/Afdelingen/Centrum-voor-Thuisbeademing/Wanneer-komt-u-in-aanmerking-voor-thuisbeademing
Slaapinfo: http://www.slaapinfo.nl/slaapstoornissen/slaapafhankelijke-ademhalingsstoornissen/slaapapneu/
Chuangshi Wang, Shrikant I Bangdiwala, Sumathy Rangarajan, Scott A Lear, Khalid F AlHabib, Viswanathan Mohan, Koon Teo, Paul Poirier, Lap AhTSE, Zhiguang Li (dec 2018)
Association of estimated sleep duration and naps with mortality and cardiovascular events: a study of 116 632 people from 21 countries. EuropeanHeart Journal, Volume 40, Issue 20, 21 May 2019, Pages 1620–1629, https://academic.oup.com/eurheartj/article/40/20/1620/5229545https://doi.org/10.1093/eurheartj/ehy695
Chaput JP; Després JP; Bouchard C; Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study fromthe Quebec Family Study. SLEEP 2008;31(4):517-523. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2279744/
Feng, P., Becker, B., Zheng, Y., Feng, T. (2017). Sleep deprivation affects fear memory consolidation: bi-stable amygdala connectivity with insula andventromedial prefrontal cortex. Social Cognitive and Affective Neuroscience, 13(2), 145-155.https://psychcentral.com/blog/how-being-sleep-deprived-alters-a-brain-connection-that-causes-fear-and-anxiety#1
Fysiotherapie en Wetenschap: http://www.fysiotherapiewetenschap.com/expert/23/zuurgraad-van-het-bloed-bij-copd, Dr. E. Elske Kusters, klinischchemicus Bronovo ziekenhuis
Medics for Medics: http://www.medics4medics.com/nl/zuurbase-evenwicht
Longziekten band II Zie hypercapnie symptomen Prof. dr.M. Demedts, Prof.dr J.H Dijkman, Prof. dr. C Hilvering, Prof. dr. D.S Postma
Helm Els , MSc, Ninad Gujar, MSc, and Matthew P. Walker, PhD (2010 ) Sleep Deprivation Impairs the Accurate Recognition of Human Emotions https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2831427/
Els van der Helm in Max Masterclass 11 november 2020:
https://www.maxvandaag.nl/programmas/tv/max-masterclass/max-masterclass/POW_04765788/
Helm, Els & Walker, Matthew. (2012). Sleep and Affective Brain Regulation. Social and Personality Psychology Compass. 6. 10.1111/j.1751-9004.2012.00464.x.
Hersenletsel-uitleg
Lin Xu, Chao Qiang Jiang, Tai Hing Lam, Bin Liu, Ya Li Jin, Tong Zhu, Wei Sen Zhang, Kar Keung Cheng, G. Neil ThomasSleep. 2011 May 1;
| Short or Long Sleep Duration Is Associated with Memory Impairment in Older Chinese: the Guangzhou Biobank Cohort Study 34(5): 575–580. Published online 2011 May 1. doi: 10.1093/sleep/34.5.575 PMCID: PMC3079936
Lin Xu, MPH, Chao Qiang Jiang, MD, Tai Hing Lam, MD, Bin Liu, Master of Medicine, Ya Li Jin, Master of epidemiology, Tong Zhu, Master ofMedicine, Wei Sen Zhang, PhD, Kar Keung Cheng, PhD, and G. Neil Thomas, PhD (2011) Short or Long Sleep Duration Is Associated with MemoryImpairment in Older Chinese: the Guangzhou Biobank Cohort Study. Sleep. 2011 May 1; 34(5): 575–580. Published online 2011 May1. doi: 10.1093/sleep/34.5.575
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3079936/
Neurology; University of California, San Diego- proefschrift van dr. Liat Ayalon (April 15, 2009) Neurology;
Saletin J. M. , E. van der Helm, Matthew Walker (2011)STRUCTURAL BRAIN MORPHOLOGY OF THE HUMAN PREFRONTAL CORTEX PREDICTS INTER-INDIVIDUAL DIFFERENCES IN NREM SLOW WAVEHOMEOSTASIS
Vaccaro Alexandro Yosef Kaplan Dor Keishi Nambara, Cindy Lin, Michael E. Greenberg, Dragana Rogulja
Sleep Loss Can Cause Death through Accumulation of Reactive Oxygen Species in the Gut (2020)https://www.medicalnewstoday.com/articles/320501#symptoms
https://www.openanesthesia.org/hypercapnia-causes/
Justine Aaronson et al. Effects of Continuous Positive Airway Pressure on Cognitive and Functional Outcome of Stroke Patients with ObstructiveSleep Apnea: A Randomized Controlled Trial