Watershed Infarction
A watershed infarction occurs when insufficient blood flows in the border area of two different watersheds (service areas) of the large cerebral arteries. It is therefore a local death of brain cells in the border areas between two watersheds. There is a greater chance of a reduction in blood flow at the smallest ends of the blood vessels.
The other name for a cerebral infarction is ischemic brain injury.
Ischemia means insufficient blood flow to organs or tissues, resulting in a shortage of oxygen and nutrients, which can cause tissue to die. Ischemic brain injury can cause diffuse nerve cell loss in the cerebral cortex.
Causes
- severe drop in blood pressure (hypotension), this can have all kinds of causes from severe dehydration to heavy bleeding.
- heavy blood loss
- severe narrowing/occlusion of the anterior and middle or the middle and posterior cerebral blood vessels
- micro-emboli; an embolism (Greek = ἔμβολος) is the occlusion of an artery or a vein
- heart attack
- serious brain infections
- sepsis: This is a serious infection that spreads in the bloodstream. Sepsis causes an extreme inflammatory reaction that can cause the
blood pressure to drop dramatically. - in case of a slowly progressive picture the cause is uncertain.
In most cases a sharp drop in blood pressure is the cause. The rarest form is caused by a hemorrhage.
The border zones of the watersheds of the following blood vessels may be involved:
- the central carotid artery (arteria carotis)
- the anterior cerebral artery (ACA)
- the middle cerebral artery (arteria cerebri media (ACM sometimes called MCA) also in the subcortical areas
- the posterior cerebral artery (PCA)
- blood vessels in the cerebellum (cerebellar arteries)
- the small arteries in the basal ganglia
See our special page on cerebral blood vessels for an explanation of these blood vessels.
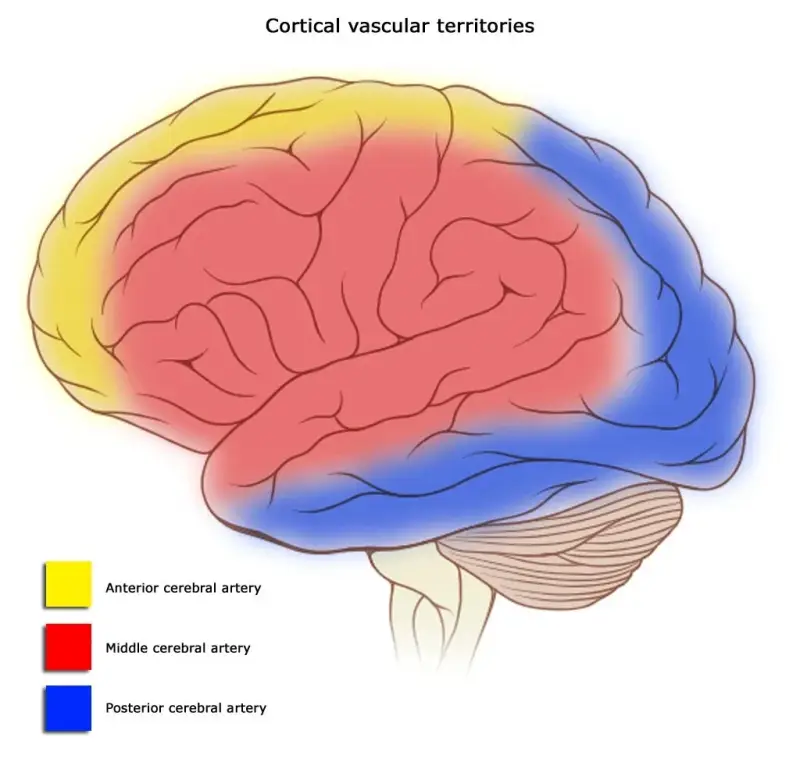
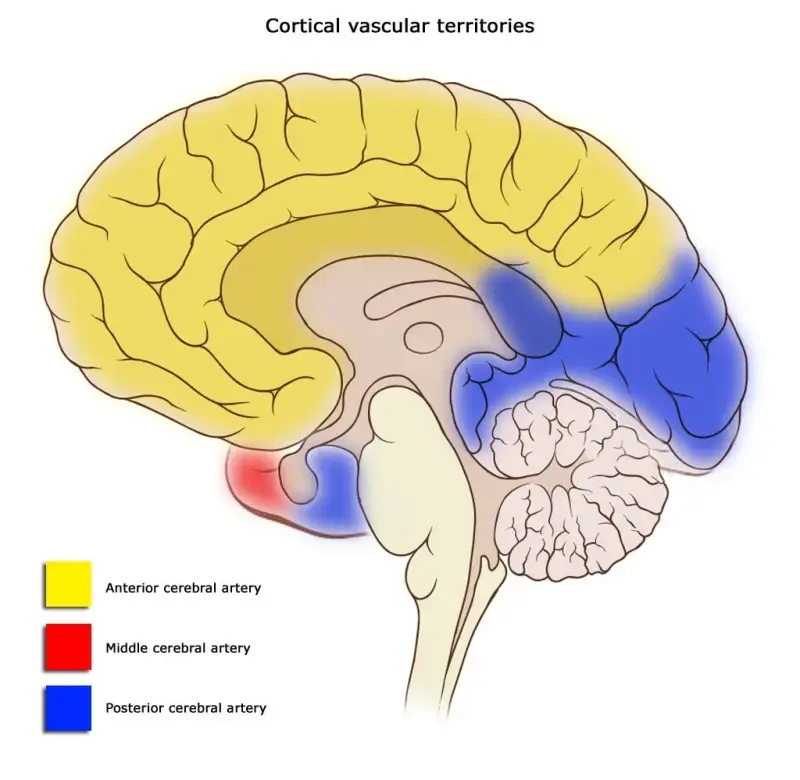
A watershed infarction can then occur at the border areas of red and yellow, or red and blue.
Red: the area supplied with blood by the middle cerebral artery, middle cerebral artery (ACM or MCA).
Yellow: the area supplied with blood by the interior cerebral artery, anterior cerebral artery (ACA).
Blue: the area supplied with blood by the posterior cerebral artery, PCA.
From the exterior Cross section
Common or rare?
- 10% of all cerebral infarctions are watershed infarctions.
- The anterior and middle cerebral arteries are most often involved in watershed infarctions, which means that the fields between these areas suffer the most from a blood flow disorder that leads to an infarction.
- Watershed infarctions caused by blood loss are the least common.
Symptoms
The symptoms that may occur depend on the affected brain area. However, because these are border areas (tissues that border the tissues that are served by the main cerebral arteries), the symptoms are often milder and are easily overlooked at first.
Transient symptoms at the start occur in 27% of people with this type of cerebral infarction. The blood flow falters, as it were, and as a result symptoms can come and go.
The symptoms may include numbness, reduced sensation and increased reflexes (hyperreflexia). Weakness or paralysis (loss of motor control) on one side, hanging the head to one side, drooping face, epileptic seizures, slurred speech, reduced vision in part of the visual field and other neurological problems can also occur.
Watershed infarctions are classified as:
- Cortical (external) border zone infarction
- between ACA (yellow in the image above), ACM (red) and PCA areas (blue)
- wedges between cortical and subcortical infarction or cortical laminar necrosis
Cortical laminar necrosis or pseudolaminar necrosis means that neurons in the cerebral cortex of the brain die (necrosis) in situations where the supply of oxygen and glucose is insufficient. This often occurs in cardiac arrest, oxygen deficiency in the tissue (hypoxia) and / or too low blood sugar (hypoglycemia).
- Deep (internal) border zone infarction
- between ACA (yellow in the image above), ACM (red) and PCA areas (blue)
- medullary, lenticulostriate, recurrent artery of Heubner and anterior choroidal arteries.
On the scans a 'rosary' pattern can often be recognized; an elongated pattern. See the images below:
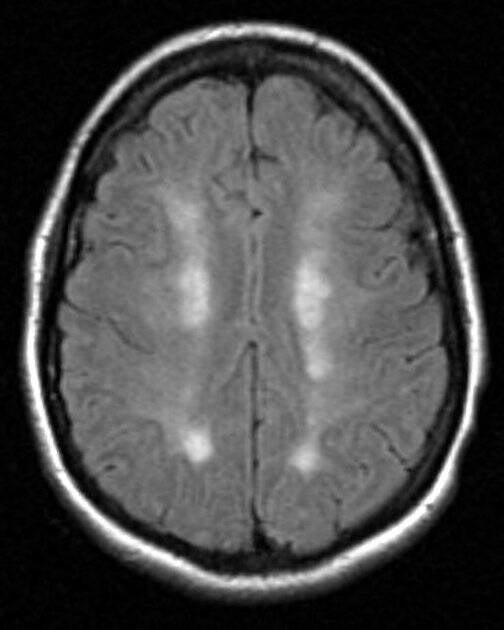
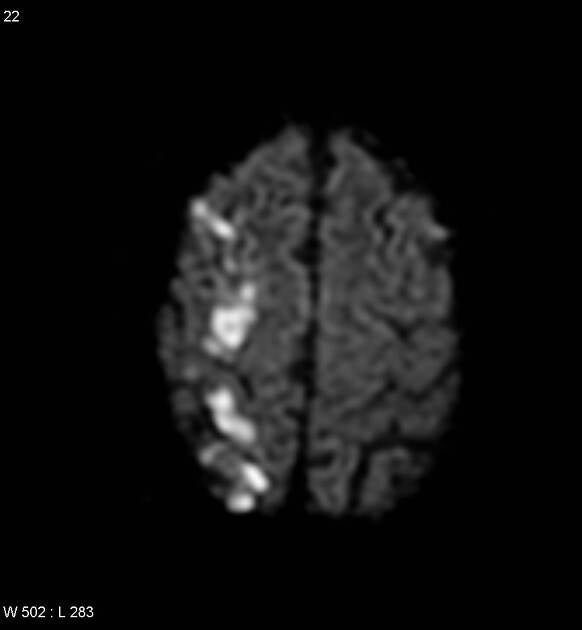
Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org. From the case rID: 2626 and the case rID: 5199
Resources
Adams J.H., Brierley J.B., Connor R.C.J., Treip C: The effects of systemic hypotension upon the human brain. Clinical and neuropathologicaJ observations in 11 cases. Brain 89: 235-268, 1966
Brierley J.B., Excell B.J.: The effects of profound systemic hypotension upon the brain of m. rhesus. Physiological and pathological observations. Brain 89: 269-298, 1966 Castaigne P, Lhermitte F, Cambier J, Gautier JC- Obstruction bilaterale des carotides internes. Etude anatomo-clinique d'une observation avec survie prolonged. Presse Med 71: 757-760, 1963
Prof Frank Gaillard, Radiopaedia.org. From the case rID: 2626 and the case rID: 5199
Hersenletsel-uitleg ~ z.d. team Hersenletsel-uitleg
Liberman AL, Zandieh A, Loomis C, Raser-Schramm JM, et al. Symptomatic Carotid Occlusion Is Frequently Associated With Microembolization. Stroke. 2017;48(2):394–399. doi: 10.1161/STROKEAHA.116.015375. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Lindenberg R., Spatz H., : Uber die Tromboendarteritis obliterans der Himgefasse (cerebrale Form der V. Winiwarter-Buergerschen Krankheit). Virchows Arch path Anat 305: 531-557, 1939
McKibbin D.W., Bullkley B.H., Green W.R., Gon W.L., Hutchins G.M. Fatal cerebral atheromatous embolization after cardiac bypass Journal of Thorac. Cardiovasc. Surgery 71: 741-745, 1976
Price D.L., Harris J. Cholesterol emboli in cerebral arteries as a complication of retrograde aortic perfusion during cardiac surgery. Neurology (Minneap.) 20: 1209-1214, 1970 Romanul F.C.A., Abramowicz A.,: Changes in the brain and pial vessels in arterial border zones. Arch Neurol 11: 40-65, 1964
Spatz H.: Uber die Beteihgung des Gehirns bei der V. WiniwarterBuergerschen Krankheit (Tromboendangiitis obliterans). Dtsch Z Nervenheilk 136: 86-132, 1935
Stehbens W.E.: Pathology of the cerebral blood vessels. C B Mosby Company, St. Louis, 1972 Torvik A., Jörgensen L.: Thrombotic and embolic occlusions of the carotid arteries in an autopsy series. Part 2. Cerebral lesions and clinical course. J Neurol Sci 3: 410-432, 1966 Torvik A., Skullerud K.: Watershed infarcts in the brain caused by microemboli. Clin Neuropath 1: 99-105, 1982
Torvik A. The pathogenesis of watershed infarct in the brain. Stroke 1984; 15: 221-3. Zulch K.J.: Die Pathogenese von Massenblutung und Erweichung unter besonderer BerOcksichtigung khnischer Gesichtspunkte. Acta Neurochir Suppl 7: 51-117, 1961
Pictures/afbeeldingen Brain to the left :This image is a derivative work of the following images: Image:Brain_stem_normal_human.svg licensed with Cc-by-2.5 + 2007-12-03T20:04:35Z AnonMoos 518x600 (78663 Bytes) == Summary == {{Information |Description = Brain and brainstem normal human diagram |Source = Trivially modified version of [[:Image:Skull and brain normal human.svg]] |Date = December 23, 2006 |Author = Patrick J. Lynch, med
Cortical areas and their arterial blood supply
derivative work: Frank Gaillard (talk) Brain_human_sagittal_section.svg: Patrick J. Lynch, medical illustrator - Brain_human_sagittal_section.svg
https://upload.wikimedia.org/wikipedia/commons/c/c0/Cerebral_vascular_territories_midline.svg