General information on causes
Brain injury is usually classified into congenital and acquired brain injury. Non-congenital or acquired brain injury is any form of brain injury that has occurred after birth. The boundary between congenital or acquired is often placed on a half-year border after birth.
For information about congenital brain injury, please visit our special page.
Acquired Brain Injury (ABI) is classified by cause:
- Traumatic and
- Non-traumatic brain injury
Some prefer the general term brain disorders.
Traumatic brain injury
Traumatic brain injury is injury that arises from the outside of the body. The following distinction is made:
- Brain injury without skull injury (for example: traffic accident, fall, heavy object against the head, blow or kick to the head)
- Brain injury with skull injury (such as the penetration of the bone due to skull fracture, penetration of an object such as bullet, stabbing weapon, iron object, etc.)
Examples of traumatic brain injury:
- Brain contusion
- Concussion and PCS
- Whiplash / WAD
- Epidural hematoma / bleeding
- Subdural hematoma / bleeding
- Shaken baby syndrome
Non-traumatic brain injury
Non-traumatic brain injury is caused by a process or condition within the body, such as:
- Stroke / cerebrovascular accident CVA
- Cerebral infarction: occlusion of blood vessel (+ many sub-forms). A stroke is caused by a narrowed or blocked blood vessel in the brain. The narrowed or blocked blood vessel prevents the brain tissue behind it from receiving nourishment and oxygen, causing that part of the brain to die.
- ADA2 deficiency DADA2
- APS-Antiphospholipid syndrome
- Avellis syndrome
- CADASIL
- Dissection
- Factor V Leiden
- Lacunar infarction
- Moyamoya syndrome MMD with infarction
- PICA syndrome
- RVCL
- Sinus thrombosis CVST or CVT
- Small Vessel Disease (SVD)
- Benedikt syndrome
- Claude syndrome
- Millard Gubler syndrome (ventral pontine syndrome)
- Parinaud syndrome
- Sneddon syndrome
- Wallenberg syndrome
- Weber syndrome
- Watershed infarction
- Cerebral infarction: occlusion of blood vessel (+ many sub-forms). A stroke is caused by a narrowed or blocked blood vessel in the brain. The narrowed or blocked blood vessel prevents the brain tissue behind it from receiving nourishment and oxygen, causing that part of the brain to die.
- Cerebral hemorrhage: blood vessel bleeding (+ many sub-forms) When a blood vessel ruptures, blood flows out, pressing on brain tissue. That area is deprived of oxygen and nutrients and dies.
- Aneurysm
- Sub Arachnoid Hemorrhage SAH
- Moyamoya syndrome MMD with cerebral hemorrhage
- Hereditary CAA or HCHWA-d
- Cerebral Amyloid Angiopathy CAA
- Arterio Venous Malformation AVM
- Cavernous malformation CCM
- ADA2 deficiency DADA2
- Dissection
- TIA: temporary closure blood vessel max 24 hours. A TIA is a mild stroke, a mini-stroke, in which a blood clot (embolism) briefly blocks an artery in the brain, causing failure. The 24-hour cut-off point is quite arbitrary. The point is that a TIA disappears after a short time, while a stroke lasts for a longer period of time.
- Infection: When the brain swells due to inflammation, the skull stops the swelling, causing the swollen brain to propel in a different direction. This allows it to press down on the brain stem. From this part of the brain, vital functions such as breathing and heartbeat are controlled. The conditions mentioned below vary in severity.
- ADEM Acute Demyelinating EncephaloMyelitis
- Brain abscess
- Covid-19 neurological consequences
- Creutzfeld-Jacob CJD
- Encephalitis
- Meningitis
- Blood poisoning / sepsis
- Legionella
- Myalgic encephalomyelitis ME
- Post-COVID syndrome / Long COVID (not necessarily a brain injury)
- Q fever (not necessarily a brain injury)
- Sepsis Blood poisoning
- Sinus thrombosis CVST or CVT (infectious form)
- White matter disorder
- Lyme disease
- Tumor (+ many sub-forms): A tumor is a growth that occurs due to uncontrolled cell division, so when body cells start to proliferate uncontrollably. This can be benign or malignant. A tumor is malignant when it spreads to other parts of the body.
- Poisoning / intoxication fetal alcohol syndrome,
solvents, heavy metals, neurotoxins
Poisoning or intoxication may be the cause of brain damage.
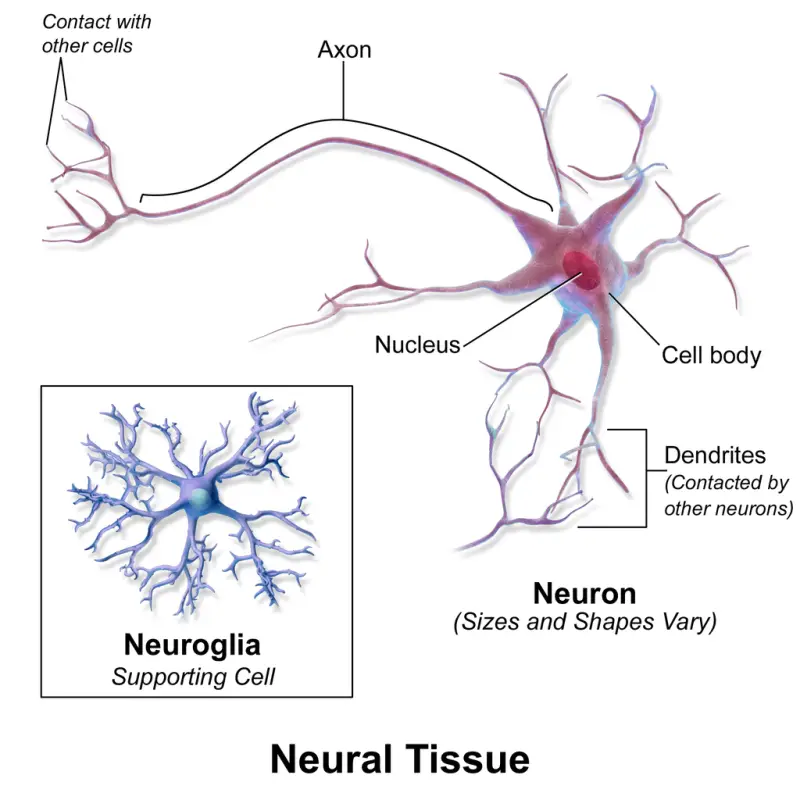
The substances that are toxic to the nervous system (neurotoxic substances) affect the functioning of neurotransmitters (substances that allow brain cells (neurons) to communicate with each other).
- Oxygen deficiency / hypoxia / anoxia (as a result of cardiac arrest / resuscitation, near drowning, trachea closure, smoke poisoning, for the child during complicating pregnancies or childbirth). The brain has an emergency energy supply of oxygen and glucose for about three minutes.
- Epilepsy may be a cause of brain injury, but may also be a result of brain injury. Epilepsy is an irritation of nerve cells in the brain tissue, sometimes accompanied by jerking movements and reduced/absent consciousness.
- Water head / hydrocephalus as a cause and also as a result of brain injury. Hydrocephalus/hydrocephaly is said to occur when the cavities (ventricles) in the brain contain more cerebrospinal fluid than they should. The skull is a closed space and too much cerebrospinal fluid increases the pressure in the brain. This pushes the brain against the skull and causes damage to the brain tissue. Brain functions may be affected.
- Degenerative diseases (neurodegenerative)
A neurodegenerative disease is a multisystem disease. This means that various bodily functions and organs can be affected, with a range of symptoms. In neurodegeneration, this is chronic in nature. Over time, sometimes years, more and more nerve cells or the connections between these nerve cells in the brain die.
- Multiple sclerosis
- ALS - Motor Neurone disease
- Parkinson
- Alzheimer's
- Huntington
- Cortico basal degeneration or CBD
- Progressive supranuclear palsy or PSP
- Frontotemporal dementia or FTD
- Lewy Body dementia
- Multiple system atrophy or MSA
- Autosomal Dominant hereditary Cerebellar Ataxia or ACDA
- Chronic Traumatic Encephalopathy or CTE
- Pregnancy complications
- pre-eclampsia
- eclampsia
- HELLP syndrome
- Locked-in syndrome
The locked-in syndrome may be caused by a hemorrhage or a heart attack, but it may also be caused by traumatic injury. Locked-in syndrome is a condition in which the patient is locked in his or her own body. He or she is aware of his or her surroundings, but can no longer move or communicate due to complete paralysis.
- Rare blood diseases
Rare blood diseases may be the cause of a cerebral infarction or cerebral haemorrhage and thus of brain damage. At the same time, severe anaemia, from a rare or not rare blood disease, can lead to oxygen deficiency in the brain and increase the chance of a cerebral infarction and cognitive complaints.
- Encephalopathy
The word 'encephalopathy' literally means disease of the brain, brain damage. Encephalopathy is a general term without naming the cause. The cause is often written before the word.
- Anoxic Encephalopathy and Postanoxic Encephalopathy
- Chronic Toxic Encephalopathy (CTE)
- Chronic Traumatic Encephalopathy
- Creutzfeld-Jacob CJD Spongiform Encephalopathy
- Hashimoto Encephalopathy /SREAT
- Hepatic Encephalopathy (HE)
- Hypertensive Encephalopathy
- Lead Encephalopathy
- Metabolic Encephalopathy
- Minimal Hepatic Encephalopathy (MHE)
- Portal Systemic Encephalopathy
- Posterior Reversible Encephalopathy Syndrome (PRES) / Reversible Posterior Leukoencephalopathy Syndrome
- Progressive Multifocal Vascular Leukoencephalopathy (PML)
- Susac Syndrome
- Toxic Encephalopathy
- Uremic Encephalopathy
- Wernicke Encephalopathy
- Anoxic Encephalopathy and Postanoxic Encephalopathy
Focal brain injury - focal pathology; in one or more places
Focal injury usually occurs after a direct blow to the head, causing a skull fracture. Often there is a bruise in the brain under the skull fracture. See our page on this.
Diffuse brain injury - diffuse pathology; spread over the brain
Diffuse injuries occur, for example, after a car accident or a fall in which the brain is shaken. This causes damage to the connections between nerve cells, which is called 'diffuse axonal damage'. This kind of damage is often spread over a larger part of the brain than a focal damage. Because a larger part of the brain is damaged, there may be more problems. See our page on this.
White matter? Gray cells?
The brain consists of white and gray matter. The white matter is located inside the brain and the gray matter is on the outside of the brain. The gray matter is the cortex around it, the cerebral cortex.
Gray matter: receiving information
The gray matter in the brain has the function of processing information.
The gray-brown color is due to the mixture of blood vessels and cell nuclei/bodies of nerve cells. The gray matter contains:
- dendrites
- short axons
- cell nucleus/cell body neurons
- supporting cells (glia cells)
The cerebral cortex therefore consists of the gray matter with the brain cells. That is why the term gray cells is used when talking about the brain. The cerebral cortex is a thin layer of two to six millimeters thick.
White matter: communicating with each other
The white matter in the brain functions to ensure communication between nerve cells. The white color comes from the myelin, the protective layer or sheath that ensures electrical conduction. The axon sends information to other brain cells and the spinal cord (the central nervous system). The different parts of the brain are thus connected to each other.
White matter damage
The brain consists of white and gray matter. The white matter is located inside the brain and the gray matter is located on the outside of the brain, the brain cells. That is why one uses the term gray cells when talking about the brain.
White matter is a white layer (myelin) that protects the foothills of the brain cells. With these spurs, the different parts of the brain are interconnected.
Damage to the small blood vessels in the brain can be observed on an MRI scan as white matter abnormalities.
The image below is from this site.
When brain cells are not able to communicate with each other, a problem arises. This problem is not always visible to the environment, but it is a (major) handicap for the person in question: brain injury with invisible effects.
There are about a hundred different white matter diseases including:
- Multiple Sclerosis
- Metachromatic leukodystrophy (MLD), a hereditary congenital metabolic disorder
- Vanishing White Matter (VWM) or CACH which stands for Cerebral Ataxia with Central Hypomyelination, a defect in the hereditary material. We discuss ataxia on a separate page.
- X-linked adrenoleukodystrophy (X-ALD), a hereditary metabolic disorder
- 4H syndrome.
- MHC (Megalencephalic leukoencephalopathy with subcortical cysts), a hereditary condition.
- Periventricular leukomalacia (PVL), a damage to the brain tissue that can occur in premature babies.
It turns out that the white matter diseases differ so much from each other that they have a specific pattern in the white matter that is made visible with an MRI brain scan.
