Dementia with Lewy bodies (DLB)
Although Dementia with Lewy bodies (DLB) is one of the most common forms of dementia, little is known about it.
DLB is a form of dementia in which so-called Lewy bodies are present in the cranial nerves.
Lewy bodies are abnormal protein deposits (clumps of alpha-synuclein) in nerve cells. This makes it more difficult for a nerve cell with Lewy bodies to transmit information to another nerve cell. Eventually, the nerve cells will die.
Researchers believe that Lewy bodies develop when a brain cell is in danger, for example when a toxic substance is present in the brain. Dementia with Lewy bodies has many characteristics of Parkinson's disease. Lewy bodies are also found in Parkinson's disease. This makes it very difficult to diagnose DLB.
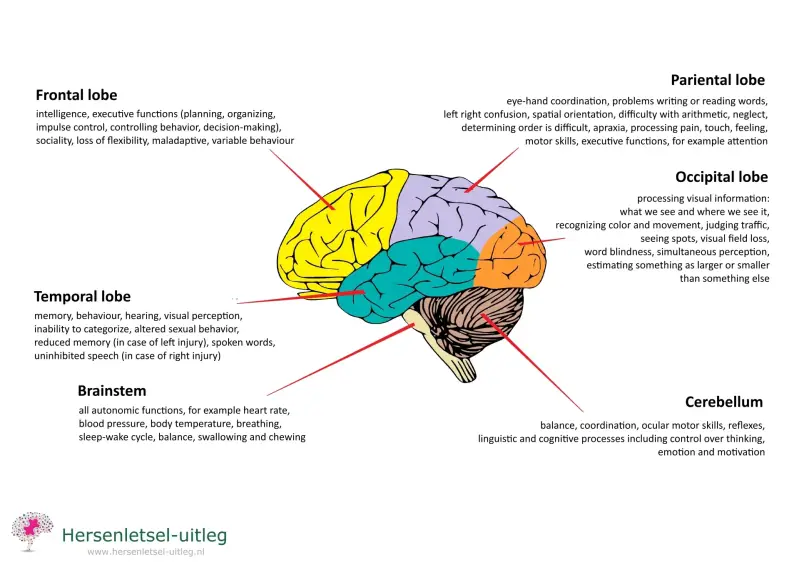
The disease begins in the black nuclei (substantia nigra) in the upper part of the brain stem. That part is called the mesencephalon or
midbrain. The disease then slowly spreads to other locations in the brain and eventually Lewy bodies are also found in the cerebral cortex.
That is why the symptoms are completely different from other forms of dementia, where the brain areas where memory is located are affected first.
That is not the case with a disease that starts in the brain stem, such as DLB. With such a disease, memory may not be impaired for a long time at first. Attention and concentration problems will be noticed sooner.
Four main characteristics
Lewy body dementia is characterized by both psychological and physical complaints.
The disease has four main characteristics and in case two of these characteristics are present, it can be said that Lewy body dementia is likely:
- changes in cognition, attention, motor skills and mood
- repeated visual hallucinations/illusions
- signs of parkinsonism
- sleep disorder (REM sleep behavior disorder)
In addition to the main characteristics, there are also probability characteristics.
Possible symptoms
- Fluctuations in symptoms
The variation in symptoms can vary from day to day. One day the person can function reasonably well, while the next moment he or she can suddenly suffer from severe confusion. There is also a strong variation in the pace of thinking, alertness, attention and memory. This is called 'varying cognition'. These symptoms can even vary from hour to hour.
In addition, the motor skills and emotions fluctuate. Someone can be happy one moment and sad or agitated the next. It also happens that someone alternates between a state of hyperalertness, normal alertness or drowsiness. It can also sometimes be difficult to make contact and you encounter someone who just stares into space. All of this makes it very difficult and frustrating to deal with the disease. This applies to both the person who has the disease and their loved ones.
- Visual hallucinations and illusions
Visual hallucinations can cause people with DLB to see things, people, children or animals when they are not actually there. Visual illusions can also cause a person to mistake things for something other than what they actually are.
Sometimes people have false beliefs that can provoke aggression and agitation. The hallucinations and illusions are often very detailed, lifelike and vivid and can be frightening and confusing. This also makes dementia difficult to recognize. The visual hallucinations cannot be attributed to medication.
The visual hallucinations make it possible to distinguish dementia with Lewy bodies from another form of dementia, frontotemporal dementia (FTD), where sound hallucinations occur in particular.
There may be periods of delirium.
- Physical complaints
The physical complaints include tremors (shaking and shaking of the hands and/or feet). In addition, people experience stiffness, problems with posture and walking. People start shuffling and have slow movements (bradykinesia). These symptoms are the same as with Parkinson's disease.
That is why we also call these complaints parkinsonism.
When diagnosing DLB it is important to recognize that these physical symptoms are not caused by Parkinson's disease, medication, or other brain damage.
The symptoms are related to problems in the production of dopamine and dopamine uptake.
Dopamine is a brain signal substance (neurotransmitter) that is produced in the black nuclei (substantia nigra) that are located in the
midbrain, and belong to the basal ganglia.
Decline of autonomic functions, typical of the brainstem
Because the brainstem is affected in dementia with Lewy bodies, complaints can arise that are related to the autonomic functions:
difficult bowel movements (constipation), urinary incontinence, sleep problems and low blood pressure when standing up / feeling light-headed (orthostatic hypotension).
Due to the orthostatic hypotension, people with Lewy body dementia fall relatively easily. Falling can also be caused by damage to the substantia nigra and basal ganglia.
- Rapid Eye Movement sleep behavior disorder (RBD)
People with LBD can suffer from REM sleep behavior disorder.
REM sleep is dream sleep. REM is an abbreviation of Rapid Eye Movement. The eyes move back and forth during dream sleep. The other muscles are slack.
In REM sleep behavior disorder, unlike normal REM sleep, the other muscles are not slack.
During dream sleep (REM sleep), a person makes movements with the arms and legs and can shout or talk.
Talking in sleep is called sleep-talking or somniloguy.
It seems that the dreams are being acted out. People have difficulty falling asleep and often feel sleepy during the day. These sleep problems often occur early in the disease process.
Often someone has injuries that he or she has inflicted on themselves during wild movements in sleep. A bed partner can also be pushed out of bed or injured during the dream of the person with this sleep disorder.
REM sleep behavior disorder as a predictor of Dementia with Lewy Bodies
In 70 to 80% of people with REM sleep behavior disorder, a neurodegenerative disorder (alpha-synuclein disorder) develops within a period of about ten to twelve years.
Dementia with Lewy Bodies falls under this neurodegenerative disorder, but also Parkinson's disease and MSA.
A REM sleep behavior disorder is called a rapid eye movement sleep behavior disorder in English, abbreviated to RBD.
A central sleep apnea disorder (CSAS) will have to be ruled out.
CCAS is a sleep disorder in which the brain stem does not sufficiently control breathing during sleep. As a result, someone has great difficulty falling asleep and is often sleepy during the day. This is a serious situation in which the
carbon dioxide can rise in the blood (hypercapnia) due to breathing far too little. This can cause drowsiness during the day.
- Cognitive decline
Thinking functions are affected early in the disease. For example, cognitive complaints such as attention and concentration problems,
confusion, difficulty maintaining an overview and reduced spatial insight. A person can then no longer orient themselves well
or estimate distances well.
Memory may initially be good for a long time. Attention and concentration problems will be noticed sooner. People with DLB can recognize someone for a long time, even if that person has not been there for a while. Problems with memory will increase later
during the disease process, in contrast to, for example, Alzheimer's disease, where memory problems are noticed sooner.
Distraction by visual stimuli is characteristic of people with DLB. The inability to separate sensory stimuli is also striking. The latter is also a characteristic of sensory overstimulation.
- Personality changes
Because Lewy bodies spread more and more in the brain and can eventually cause brain cells to die, personality changes can occur. Personality changes will differ per person. This depends on the area where the damage occurs, but also on the stage of the disease and the person themselves.
- Behavioural problems and mood problems
The Centre for Consultation and Expertise (CCE) mentions the following behavioural problems: "shouting, screaming, arguing, being suspicious, wanting to be right and harming oneself."
These complaints and rapid changes in mood are often noticeable early in the disease process. People with dementia with Lewy bodies can also develop depression.
- Aphasia
Aphasia is a language disorder that makes speaking, writing and understanding language more difficult. DLB can go hand in hand with the development of aphasia. The language problems are not prominent at the beginning of the disease, but only occur later.
- Hypersensitivity to antipsychotics or antidepressant medication
Many people with Dementia with Lewy Bodies are hypersensitive to the side effects of antipsychotics: medicines against hallucinations such as haloperidol. This medicine is often given also because of the restlessness. This makes treating these complaints very difficult.
Due to the hypersensitivity to this medication, existing complaints can worsen or new complaints arise such as:
- a reduced consciousness
- a strong reduction in mental functions
- immobility of the body
- disruption of autonomic functions: an increased heart rate, fluctuating blood pressure, salivation, increased body temperature and heavy sweating.
Serious reactions often occur within two weeks after administering of these medicines or after a change in dosage. These antipsychotics must then be discontinued.
Medication with central anticholinergic action, such as tricyclic antidepressants or oxybutin should be avoided as much as possible. This medication can actually cause a reduced cognitive function, hallucinations, urinary retention (urine remains in the bladder with the risk of bladder infection!), reduced breathing and a reduced blood pressure (with the risk of falling!).
Diagnosis
Making a diagnosis is difficult and can sometimes take a long time. The course of the disease can be different for everyone with Lewy bodies disease, depending on the areas of the brain that are affected and the personal circumstances.
As mentioned before, the symptoms of dementia with Lewy bodies are very similar to Parkinson's disease.
In order to make a distinction, the following rule is applied:
If a person is diagnosed with Parkinson's disease and develops symptoms of dementia within one year, it is classified as dementia with Lewy bodies. If these symptoms of dementia occur later, it is classified as Parkinson's dementia.
See the diagram of the differences between Alzheimer's disease, Parkinson's disease and dementia with Lewy bodies via
this Dutch website.
A clear distinction must be made between the different diseases because some medications can have an opposite effect.
Please also check the following websites:
EEG
For the diagnosis of Lewy Body dementia, an EEG (a brain film of the electrical activity in the brain) can also be a tool.
- With Dementia with Lewy Bodies, a severe diffuse (widely spread) delay is often seen on an EEG. These are slow waves.
Sometimes a frontal intermittent rhythmic delta activity (FIRDA) is seen. - With Alzheimer's disease, a less severe diffuse delay is usually seen.
- With FTD (frontotemporal dementia) a normal or slightly abnormal EEG is usually found
Intervention through improved diagnosis
If there is a good diagnosis, the quality of life can be improved by the right treatment.
Check whether two of the four main characteristics mentioned are present.
Are there changes in cognition, attention, motor skills and mood?
Are there Parkinson's-like symptoms?
Are there sleep disorders, changing forms of alertness, optimal alertness, drowsiness or hyperalertness with restlessness.
Check whether there is restlessness due to multiple sensory stimuli.
If the person possibly suffers from sensory overstimulation, then
reducing sound stimuli is a necessity. Then a "cozy" living room is a source of restlessness and a co-cause of sleep problems. Check whether sounds can be confusing or frightening. Are there visual hallucinations?
If a person thinks that the wife or mother is present in the room at night, recognize that and name it to health care workers as a hallucination because that is one of the main characteristics of Lewy body dementia.
Do not fight when a person is agitated or suspicious and do not try to prove that the illusions are not real. Do not repeatedly correct the person when you think something is wrong. This only worsens the agitation.
Offer peace, safety, friendliness, a ‘safe’ home layout and a predictable, orderly, clear structure in daily life and at night. Someone needs to build up sufficient energy through good sleep. Make sure the person is pain-free.
Do not judge someone for their negative behavior.
The goal is to stretch optimal alertness during the day and improve sleep/sleep hygiene.
Search for support
There are Facebook groups for people with DLB and their caregivers.
For example in Georgia (USA).
Advanced knowledge
The depression that can occur in people with DLB can be traced back to the damaged dopamine-producing nerve cells in the brainstam (substantia nigra in the midbrain / basal ganglia).
Dopamine is a neurotransmitter that gives a good feeling, for example after exertion, exercise, a difficult task, etc.
Dopamine also works to motivate and has an influence on cognition, attention, learning ability and memory and sleep.
There is partly a reduced production visible in people with dementia with Lewy bodies, but in addition there is often a reduced dopamine uptake. This is particularly visible on DaT scans in the striatum (in the basal ganglia). A DaT scan is a special SPECT scan that makes the distribution of dopamine in the brain visible.
Anyone who has the right knowledge of or reads up on the function of the brainstem (particularly the mesencephalon in the upper part of the brainstem) and the basal ganglia will recognize many complaints and hopefully be less likely to judge people with DLB.
Please check the image below.
Resources
© Hersenletsel-uitleg
Ballard, C., Grace, J., McKeith, L., & Holmes, C. (1998). Neuroleptic sensitivity in dementia with Lewy bodies and Alzheimer’s disease. The Lancet, 351(9108), 1032–1033. https://doi.org/10.1016/s0140-6736(05)78999-6
Bentley, A., Morgan, T., Salifu, Y., & Walshe, C. (2021). Exploring the experiences of living with Lewy body dementia: An integrative review. Journal of Advanced Nursing, 77(12), 4632–645.https://doi.org/10.1111/jan.14932
Braam, S., & Ten Veldhuis2, M. (2008, 20 oktober). Lewy Body: de vergeten dementie. Innovatiekring Dementie - IDé. https://www.innovatiekringdementie.nl/a-176/lewy-bodies-de-vergeten-dementie
Gouw A. en Stam. C.J., EEG bij geheugenstoornissen, Korte les KNF. Nervus - Jaargang 1 - editie 4 - 2016-4https://www.nervus-online.nl/tijdschrift/editie/artikel/t/eeg-bij-geheugenstoornissen Consulted 21 december 2022
Hayder, A., Spurling, B. C., & Sanchez-Manso, J. C. (2021, 12 juli). Lewy Body Dementia. https://www.ncbi.nlm.nih.gov/books/NBK482441/. Consulted 21 december 2021, of https://pubmed.ncbi.nlm.nih.gov/29494048/
HERSENLETSEL-UITLEG
Jellinger, K. A., & Korczyn, A. D. (2018). Are dementia with Lewy bodies and Parkinson’s disease dementia the same disease? BMC Medicine, 16(1). https://doi.org/10.1186/s12916-018-1016-8
Jonker, C. (1997). Dementie. Een visie op recente ontwikkelingen. Vrije Universiteit Amsterdam. https://research.vu.nl/en/publications/dementie-een-visie-op-recente-ontwikkelingen
Khotianov, N., Singh, R., & Singh, S. (2002, 1 januari). Lewy body dementia: Case report and discussion. ResearchGate. Geraadpleegd op 21 december 2021, van https://www.researchgate.net/publication/11520179_Lewy_body_dementia_Case_report_and_discussion
Lewy body dementie. (z.d.). Alzheimer Nederland. https://www.alzheimer-nederland.nl/dementie/soorten-vormen/lewy-body-dementie
Medische informatie. (2017, 20 september). Lewy body dementie. https://www.lewy.nl/medische-informatie/
Sanford, A. M. (2018). Lewy Body Dementia. Clinics in Geriatric Medicine, 34(4), 603–615. https://doi.org/10.1016/j.cger.2018.06.007
Taylor, J. P., McKeith, I. G., Burn, D. J., Boeve, B. F., Weintraub, D., Bamford, C., Allan, L. M., Thomas, A. J., & O’Brien, J. T. (2020). New evidence on the management of Lewy body dementia. The Lancet Neurology,19(2), 157–169. https://doi.org/10.1016/s1474-4422(19)30153-x
Wat is Lewy body dementie (LBD). (z.d.). https://www.dementie.nl/over-dementie/soorten-dementie/lewy-body-dementie/wat-is-lewy-body-dementie-lbd
Zweig, Y. R., & Galvin, J. E. (2014). Lewy body dementia: the impact on patients and caregivers. Alzheimer’s Research & Therapy, 6(2), 21. https://doi.org/10.1186/alzrt251 EEG picture: CC BY-SA 2.0, https://commons.wikimedia.org/w/index.php?curid=845554