Basal ganglia
The brain works together as one whole. Brain functions are spread throughout the brain areas and arise from the exchange between the areas. However, complaints can be identified per brain area.
The basal ganglia are also called the basal nuclei (nuclei basales) or deep nuclei
The word ganglion refers to a group of nerve cells with the same function. Ganglia is plural of ganglion.
The basal ganglia are not an anatomical unit. It is a group of five cores with the same function that are closely connected to each other. Some authors choose to distinguish nine nuclei as basal ganglia.
The basal ganglia contains a number of nuclei that control balance, posture, eye movements and initiation and regulation of movements. They are strongly connected to other motor areas in the brain, connecting the thalamus to the motor cortex.
Together with the cerebellum, the basal ganglia are also called the extrapyramidal system.
The basal ganglia organizes automatisms in movements, such as driving a car, cycling, knitting, standing upright (keeping balance) and walking. In adults, the postural reflexes are stored here.
The basal ganglia are involved in stimulation and learning of simple processes and in cognition and emotion. They play important role in motivation, desire for reward, 'reward and reinforcement' of behavior, 'response to stimulus', addictive behavior and habit formation.
The basal ganglia may also contribute to the neuropathology of depression, particularly in relation to the limbic system. In people with schizophrenia, cognitive disorders, such as memory problems and learning delays, have been linked to damage in the basal ganglia.
|
Brief summary
|
Where in the brain?
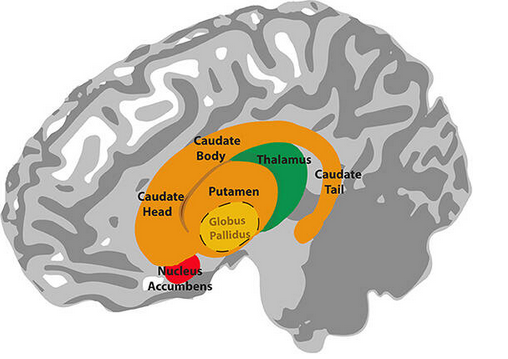
The basal ganglia or deep nuclei consist of several units that function together. Even though they are not anatomically in one place in the brain, the basal ganglia are interconnected with many pathways, forming a strong functional unit. The brain areas that belong to the basal ganglia are located fairly centrally in the brain.
The five basal nuclei (ganglia) are formed by:
- Striatum dorsal
- 1) Caudate nucleus /Nucleus caudatus (tail nucleus)
- 2) Putamen
- 3) Globus pallidus
- 4) Subthalamic nucleus
- 5) Black core (substantia nigra).
NB! Putamen and Globus pallidus together is Lentiform nucleus.
Lateral view of the basal ganglia structures:
Cross section of the brain showing basal ganglia. The tegmentum is part of the midbrain; the upper part of the brainstem.
There is the substantia nigra located.

Anatomy and function of the subregions of the basal ganglia
Corpus striatum
The corpus striatum literally means 'the striped body' and can be divided into:
1. Striatum dorsale (dorsal side) with two parts:
- Putamen is involved, among other things, in the regulation of motor skills, both voluntary and involuntary movements. It helps the limbs
prepare for movement and helps with movement. Furthermore, the putamen is involved in learning and motor control of speech, such as
speech articulation (speech apraxia and dysarthria). The putamen is also necessary for language functions, reward, cognitive functioning and addiction.
A wide spectrum of movement disorders, cognitive and psychiatric disorders can result from injury in the putamen.
It can result in involuntary, jerky muscle movements or tremors such as in Huntington's disease. Parkinson's disease is the result of dopamine deficiency in the posterior putamen and is characterized by stiffness, tremors, ataxia and disturbance of balance.
Restless legs syndrome can also be a result of injury to the putamen. Restless legs syndrome causes jerking of the legs and a painful urge to move the legs.
Furthermore, the following diseases are associated with damage to the putamen: Alzheimer's disease, Lewy body dementia, obsessive compulsive disorder (OCD), bipolar disorder, Tourette syndrome, and ADHD; attention deficit hyperactivity disorder. A decrease in putamen volume is seen in major depressive disorder, Williams syndrome, autism and schizophrenia.
The putamen and the globus pallidus together form, anatomically (not in terms of function), the lens nucleus or the lentiform or lenticular nucleus.
Image of the putamen:

- Nucleus caudate / caudate nucleus (tail nucleus) has the shape of an elongated C in both hemispheres. It has the following functions:
- transmitting all kinds of sensory information about the spatial position of the body
- regulating the posture of the body, arms and legs
- controlling accuracy of movements
- controlling the speed of movements
- short- and long-term memory storage
- language processing
- ability to learn
- receiving feedback
- motivation and desire for reward
The information runs through the putamen and the globus pallidus to the thalamus, after which it ultimately ends up in the frontal cerebral cortex (cortical
areas).
Recent research showed that changes in the caudate nucleus, may explain the fatigue in Multiple Sclerosis and traumatic brain injury. Functional brain scans have shown connections with the areas in the cerebral cortex that become active in executive functions such as inhibitory control, decision-making and planning.
Image of the nucleus caudate / caudate nucleus

2. The striatum ventrale (on the ventral side)
This ventral part is considered part of the limbic system.
- Nucleus accumbens forms part of the brain's reward circuitry and behavioral mediation.
- Olfactory tubercle (tuberculum olfactorium) is part of the olfactory tract for odor perception.
Certain parts of the caudate nucleus and the putamen are also included in the striatum ventrale.
Globus pallidus
The globus pallidus (paleostriatum or pale sphere and also known as dorsal pallidum) regulates motor functions, influences learning functions and uses dopamine that is produced in black core (substantia nigra).
It sends information from the basal ganglia to the thalamus through the neurotransmitter gamma aminobutyric acid (GABA), which has an inhibitory effect on motor function.
The globus pallidus can be damaged by carbon monoxide poisoning, oxygen deficiency (hypoxia), poisoning with severe sleep and sedative barbiturate (barbiturate intoxication), cyanide poisoning, hydrogen sulfide poisoning, severe long-term low blood sugar levels (hypoglycemia), low blood pressure (hypotension) and copper overload in the body; Wilson's disease.
Damage to the globus pallidus affects learning functions and movement disorders.
Image of the Globus pallidus

Lentiform or lenticular nucleus (lens nucleus)
The putamen and the globus pallidus together form the lens nucleus or the lentiform or lenticular nucleus. It gets its name from its shape of a lens.
The globus pallidus forms the conical part of the lentiform nucleus for which the putamen forms a cap.
There is no functional unit, only an anatomical connection. They are separated by a thin layer of white matter; the medial medullary lamina.
The lens nucleus is described in various conditions,
such as atypical parkinsonian syndromes (MSA, PSP), Wilson's disease (copper overload) and dystonia.
Subthalamic nucleus
The subthalamic nucleus or subthalamic nucleus (Luys' bodies) includes:
- Dorsal (motor) part, which receives input from the primary motor cortex.
- Ventrolateral (associative) part, which receives input from the prefrontal cortex and frontal eye fields.
- Ventromedial (limbic) part, which receives input from the anterior cingulate cortex.
The subthalamic nucleus is involved in voluntary and involuntary movements, associative learning and limbic functions.
For the movement disorders that can occur due to damage to the subthalamic nucleus, see the bottom of this page.
Black core / Substantia nigra
The black nucleus or substantia nigra is located in the front part of the mesencephalon (midbrain) and supplies the basal ganglia with dopamine. It is a motor nucleus. Despite its location in the mesencephalon, it is considered part of basal ganglia in function. The black nucleus is involved in voluntary movements, orientation in space, learning, mood regulation, and activity related to the reward circuit of the brain.
It consists of:
- The pars compacta (SNc) on the dorsal side with melanin-filled neurons. Melanin is the dark color (pigment) that gives the black core its name. It supplies the striatum with dopamine and is very important for transmitting signals from the basal ganglia to the thalamus. It is involved in motor control and coordination. From the substantia nigra, nerve pathways run to the striatum (striped body). This is called the nigrostriatal pathway.
The loss of dopamine neurons in this part (SNc) appears to be responsible for the development of Parkinson's disease and some other parkinsonian syndromes.
Dopamine is a signaling substance (neurotransmitter) that is related to movement disorders, psychiatric disorders and behavioral problems.
Read more about dopamine via this link. - The pars reticulata (SNr) on the ventral side is important in the regulation of eye movements.
Injury to parts of the basal ganglia
Damage to the basal ganglia can be caused by various types of brain injury, including cerebral hemorrhage, cerebral infarction, tumor or silent cerebral infarction (SCI) that goes unnoticed except during an accidental brain scan.
Movement disorders
The consequences of damage to the basal ganglia can be the following movement disorders:
- Ataxia is a balance and coordination disorder, a movement disorder. Balance and coordination of movement are affected.
A person with ataxia has an uncertain gait and moves his arms, legs and torso in a 'jerky' and uncontrolled manner. - Athetosis is characterized by continuous, slow, involuntary movements of fingers, hands, feet and toes, sometimes arms, legs, neck and tongue. The fingers are often overextended. The joints writhe or contort continuously or while rolling slowly. When the facial muscles move, the face appears to be grimacing. The neck muscles appear thickened (hypertrophy) because the neck muscles contract frequently and the head then turns.
- Ballism (proximal chorea) is characterized by involuntary, lurching irregular, coarse movements. It is related to chorea but the movements in ballism are slower than in chorea. Ballism often involves, as the name 'proximal chorea' indicates, proximal body parts. Proximal means closer to the center of the body than any other part of the body. In the case of ballism, it concerns the hip, thighs, upper arms and shoulders. The hip joint is located proximal to the knee joint. The upper arms lie proximal to the forearms.
Ballism is often caused by damage to the subthalamic nucleus, which is part of the basal ganglia.
Globus pallidus, Putamen or Caudate nucleus, the other parts of the basal ganglia, can also be disturbed.
During sleep the movements may calm down, but when aroused, the movements become stronger. Causes of ballism can be: bleeding, an infarction, a tumor or metastasis (spread) or an infection.
If it occurs on one side of the body, it is called hemiballism.
The term 'Ballism' is derived from the Greek word for throwing and swinging. Ballism is one of the hyperkinetic movement disorders. The term 'hyperkinetic' means: with excessive energy.
See the video under hemiballism. Hemiballism is ballism on one side of the body.
- Bradykinesia is characterized by a general slowness of movement and is the most common form of reduced movement
(hypokinesia). For example, a person may move back and forth in the chair a few times before he or she can get up. Automatic movements, such as blinking the eyes, are less fast and smooth. This occurs, for example, in Parkinson's disease, other conditions and due to old age.
- Chorea is characterized by sudden, irregular, involuntary, undirected (purposeless), continuous, 'dance-like', sometimes graceful movements of the face, hands, arms, neck or torso. The movements may last for several seconds to minutes and are not rhythmic in nature. The movements cannot be suppressed and there is no urge to move. 'Chorea' is the Greek word for dance. It is caused by injury in the Red Nucleus or by injury in the basal ganglia. There are several diseases in which chorea occurs, but the most characteristic is Huntington's disease. This involves degeneration of striatal GABA neurons, causing the head of the Caudate nucleus to become smaller (atrophy).
- Dystonia is characterized by involuntary, persistent muscle contractions; spasms in muscles or muscle groups.
This can cause repetitive or twisting movements or an unnatural position of the body part. The often painful movements are often accompanied by a tremor.
Forms of dystonia can be classified by cause, age of onset, or by distribution over the body.
It may involve single muscle groups (focal dystonia), for example in spasmodic torticollis, or multiple muscle groups (generalized dystonia: extensive dystonia). Then one or both legs, the trunk and at least one other body part are involved.
In spasmodic torticollis (Cervical dystonia) there is a dystonia of the neck and neck muscles. If the head is crooked, it is called laterocollis. When the neck is turned to one side, this is called rotational torticollis. When the head is turned backwards, this is called retrocollis.
The eyelids may remain closed in a cramp. That's called blepharospasm; literally 'eyelid contraction'.
Furthermore, further divisions can be made into segmental (dystonia concerns two adjacent body parts), hemidystonia (dystonia concerns one half of the body, usually due to brain damage) and multifocal (in a number of body parts that are not adjacent to each other).
Symptoms of dystonia may include:
- Abnormal posture of the neck, toes, hands or other parts of the body.
- Involuntary turning of the neck when tired or stressed.
- Uncontrollably rapid blinking of the eyes.
- Spasms of the eyelids causing the eyelids to remain closed.
- Cramp in the foot or the tendency of a foot to turn over after walking.
- Problems with writing that cause handwriting to deteriorate after writing a few lines.
Dystonia is one of the conditions that can follow damage to the basal ganglia.
Dystonia can also have a genetic cause.
More information on dystonia can be found on Dystonia UK and on Dystonia Medical Research Foundation.
- Hemiballism is characterized by wild, involuntary, lurching, coarse movements of the limbs on one side of the body.
It is related to chorea but in ballism the movements are slower than in chorea. Ballism is often caused by damage to the subthalamic nucleus, which is part of the basal ganglia.
The Globus pallidus, Putamen, Caudate nucleus, other parts of the basal ganglia can also be disturbed.
During sleep the movements may calm down, but when aroused the movements become stronger. Causes of ballism include: bleeding, an infarction, a tumor or metastasis or an infection.
See more information above under Ballism.
- Hemiballismus-hemichorea (HBHC) syndrome is a rare hyperkinetic movement disorder.
Characteristic are involuntary, irregular, continuous, unilateral movements of the body. It is caused by damage to the basal ganglia due to a cerebral infarction, cerebral hemorrhage,
autoimmune diseases. Although rare, high blood sugar (hyperglycemia) is another possible cause of HBHC syndrome, also known as chorea-hyperglycemia-basal ganglia syndrome.
The diagnosis can be made if there are three abnormalities: chorea, high blood sugar (hyperglycemia) and radiological abnormalities
in a specific part of the basal ganglia, namely the striatum.
- Hemichorea is chorea on one side of the body. See above under Chorea.
- Hyperkinetic movement disorders are characterized by excessive and involuntary increased muscle activity, such as in Huntington's disease. They are involuntary excessive normal and abnormal movements. Sometimes accompanied by athetosis, ballism, trembling and/or chorea.
- Myoclonus is a short-lived, jerky, involuntary and usually arrhythmic (sometimes rhythmic) movement, with the same movement over and over. There is no urge to move. A myoclonus cannot be suppressed. The word 'myoclonus' comes from the words 'myo' meaning muscle and 'clonus' meaning shock. It can occur as an innocent muscle contraction, but also in epilepsy syndromes in addition to absence seizures and tonic-clonic seizures. They are called subcortical myoclonies if they occur through subcortical (located below the cerebral cortex) areas of the brain, such as the basal ganglia.
Myoclonias may be caused by genetic disorders, metabolic diseases, brain disorders (encephalopathy) caused by poorly functioning kidneys, liver, thyroid or by COVID-19. Myoclonias may also be caused by brain injury, for example: traumatic brain injury, brain inflammation/encephalitis, autoimmune inflammation of the brain, cerebral infarction/ischemic stroke and oxygen deficiency (hypoxic-ischaemic encephalopathy/HIE). Finally, myoclonias can be caused by medications. Myoclonias can also occur alongside other movement disorders, such as ataxia, dystonia or chorea.
- Tremors are characterized by abnormal involuntary, rhythmic movements of the hand, head or other body parts.
- Tics are sudden, brief, rapid and recurrent, non-rhythmic and stereotypic semi-voluntary motor movements lasting seconds. There is an urge to move. Tics always occur in the same movement. There may be multiple tics. The tics can be suppressed for a short time and are therefore called semi-voluntary movements. In particular the Striatum, part of the basal ganglia, plays a role.
In the condition PANDAS, children develop tics after experiencing a streptococcal infection (for example, after a throat infection or wound).
The tics are then accompanied by behavioral disturbances. Tics can also be caused by medications. This website has extensive information on PANDAS.
Parkinsonism
The combination of postural problems associated with damage to the basal ganglia is called parkinsonism because they are reminiscent of Parkinson's disease.
- changed movement pattern, slowed movement
- difficulty speaking, word-finding problems
- difficulty with posture and movements
- tremors; shaking, shaking and trembling
- involuntary movements, spasms
- increased muscle tension, muscle stiffness
- abnormal body position
- difficulty with balance and difficulty walking
- difficulty seeing due to inability to control eye movement
- difficulty starting a movement, keeping it going and stopping a movement
- uncontrolled repetitive movements such as in tics, also in uttering cries.
There are many diseases that resemble the symptoms of Parkinson's disease. The conditions that resemble Parkinson's disease are called atypical parkinsonisms.
Atypic parkinsonisms include vascular parkinsonism and multiple system atrophy (MSA) and progressive supranuclear palsy (PSP).
Spasticity is not one of the consequences of damage to the basal ganglia. Read about spasms and spasticity.
The following conditions and conditions involve the basal ganglia:
- Drug overdose
- Brain injury/stroke
- Brain inflammation/encephalitis
- Syphilis
- Tuberculosis
- Metabolic problems
- Poisoning with copper, manganese, lead, or other heavy metals
- Tumors
- Dystonia
- Corticobasal degeneration
- Huntington's disease; degeneration occurs of striatal GABA neurons, causing the head of the Caudate nucleus to become smaller (atrophy). This is accompanied by involuntary movements, see chorea
- Multiple System Atrophy MSA
- Parkinson's disease; the basal ganglia no longer receive dopamine from the substantia nigra, causing the patient to become increasingly impaired
to move. - Progressive Supranuclear Palsy PSP
- Wilson's disease
- Lewy body dementia
- Cerebral Palsy
- Liver disease
- Carbon monoxide poisoning
- Side effects of medications
Resources
©Hersenletsel-uitleg
Basal ganglia dysfunction. (z.d.). Medlineplus. https://medlineplus.gov/ency/article/001069.htm
Bhagwat NM, Joshi AS, Rao G, et al. Uncontrolled hyperglycaemia: a reversible cause of hemichorea–hemiballismus. Case Rep. 2013;2013:bcr2013010229.
https://jmedicalcasereports.biomedcentral.com/articles/10.1186/s13256-022-03577-3#ref-CR2
Blausen, B. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine, 1(2). https://doi.org/10.15347/wjm/2014.010 Picture By BruceBlaus.Blausen.com staff (2014). "Medical gallery of
Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. - Own work, CC BY 3.0,
Cecil, R. L. F., Goldman, L., & Schafer, A. I. (2012). Goldman’s Cecil Medicine,Expert Consult Premium Edition -- Enhanced Online Features and Print, Single Volume,24. Elsevier Gezondheidszorg.
Daroff, R. B., Jankovic, J., Mazziotta, J. C., Pomeroy, S. L., & Bradley, W. G. (2016). Bradley’s Neurology in Clinical Practice (6de editie). Elsevier Gezondheidszorg.
Eyskens, E., Deen, H. M., Feenstra, L., Meinders, A. E., & Vandenbroucke, J. P. (1997). Codex medicus (10de editie). Elsevier Gezondheidszorg.
Ghandili, M., & Munakomi, S. (2021). Neuroanatomy Putamen. StatPearls Publishing LLC.
Grahn, J. A., Parkinson, J. A., & Owen, A. M. (2009). The role of the basal ganglia in learning and memory: Neuropsychological studies. Behavioural Brain Research, 199(1), 53–60.
https://doi.org/10.1016/j.bbr.2008.11.020
Hersenletsel uitleg | Hersenletsel-uitleg.nl. (z.d.). https://www.hersenletsel-uitleg.nl/. https://www.hersenletsel-uitleg.nl/
Kéri, S. (2008). Interactive memory systems and category learning in schizophrenia. Neuroscience & Biobehavioral Reviews, 32(2), 206–218. https://doi.org/10.1016/j.neubiorev.2007.07.003
Kuks, J. B. M., Snoek, J. W., Oosterhuis, H. J. G. H., & Fock, J. M. (2003). Klinische neurologie (15de editie). Bohn Stafleu van Loghum.
Lentiform Nucleus - an overview | ScienceDirect Topics. (z.d.). Https://Www.Sciencedirect.Com/. https://www.sciencedirect.com/topics/neuroscience/lentiform-nucleus
Life Science Databases. (2009, 25 september). Caudate nucleus [Illustratie]. Wikimedia. https://commons.wikimedia.org/w/index.php?curid=7894172 次のアドレスからこのファイルで使用している画像を取得で
きますURL., CC BY-SA 2.1 jp, https://commons.wikimedia.org/w/index.php?curid=7894172
Lim, S. J., Fiez, J. A., & L.L.H. (2014, 1 augustus). Anatomy of the basal ganglia [Illustratie]. wikemedia.org. https://commons.wikimedia.org/wiki/File:Anatomy_of_the_basal_ganglia.jpg
Merchut, M. P. (2011, 30 juni). Disorders of the Basal Ganglia. PDF. http://www.stritch.luc.edu/lumen/MedEd/neurology/Disorders%20of%20the%20Basal%20Ganglia.pdf Postle, B. R., & D’Esposito, M. (1999). Dissociatie van menselijke caudate nucleus-activiteit in ruimtelijk en niet-ruimtelijk werkgeheugen: een gebeurtenisgerelateerd fMRI-onderzoek. Cognitive Brain
research., 8(2), 107–115.
Stathis, P., Panourias, P. G., Themistocleous, M. S., & Sakas, D. E. (2007). Connections of the basal ganglia with the limbic system: implications for neuromodulation therapies of anxiety and affective
disorders. Acta Neurochir Suppl, 97, 575–586. https://doi.org/10.1007/978-3-211-33081-4_67
Van Wijk, R., & Van Nieuwenhuijze, O. (2010). Jaarboek Integrale Geneeskunde 2007. https://www.bol.com/nl/nl/b/tijdschrift-integrale-geneeskunde-stich/13692921/.
Wylie, G. R., Dobryakova, E., DeLuca, J., Chiaravalloti, N., Essad, K., & Genova, H. (2017). Cognitive fatigue in individuals with traumatic brain injury is associated with caudate activation. Scientific Reports,7(1). https://doi.org/10.1038/s41598-017-08846-6
Yatsu, F. M. (2004). Neurology in Clinical Practice: The Neurological Disorders, 4th ed. Neurology, 62(9), 1657.2-1657. https://doi.org/10.1212/wnl.62.9.1657-a