Brain injury caused by a stroke - CVA
On this page we explain the different types of stroke. You can also read how you can recognize a stroke and what the consequences are of a stroke.
Table of contents
- Multiple forms of stroke
- Stroke
- Cerebral infarction
- TIA
- Sinus thrombosis
- Vascular wall problems
- Differences between cerebral hemorrhage, cerebral infarction and TIA
- Damage on the right or on the left?
- Recognize a stroke quickly / how do I recognize a stroke?
- Atypical stroke CVA complaints
- Consequences of a stroke
- Blood vessels involved
- Stroke risk factors
- Rare blood diseases
- Stress and high blood pressure as causes
- Genetic Causes
- Silent cerebral infarction SCI (unnoticed cerebral infarction or silent cerebral infarctions)
- Young stroke
1 Multiple forms of stroke
A stroke, also called CVA, stroke or attack, always has to do with an acute problem with the blood flow to the brain. This could be due to a cerebral hemorrhage or a cerebral infarction.
Of all strokes approximately:
- 80% is a cerebral infarction
20% is a stroke
The collective name CVA is an abbreviation for Cerebro Vascular Accident, i.e. a accident in the blood vessels of the brain.
Why a cerebral hemorrhage or cerebral infarction is so dangerous
In both a cerebral infarction and a cerebral hemorrhage, too little blood flows to part of the brain.
That part of the brain does not receive enough oxygen and nutrients and can die. The symptoms of failure are often the same, such as a paralyzed arm, crooked mouth and difficulty speaking.
Apoplexy (apoplexia cerebri or ictus cerebrale) is a synonym for stroke.
The more brain tissue is damaged, the more serious the consequences of a stroke.
A consequence is almost always half-sided paralysis.
Damage to the right hemisphere of the brain causes a left-sided paralysis.
Damage in the left half causes a paralysis on the right side of the body.
Why it is important to know whether it is a hemorrhage or a blocked blood vessel
The difference between a cerebral hemorrhage and a cerebral infarction is especially important for rapid treatment.
In the case of a cerebral infarction, the doctor can, within the first four and a half hours after the infarction, administer anticoagulant medications (thrombolysis, platelet aggregation inhibitors or sometimes anticoagulants) to try to reduce the size of the infarct.
But these medications are actually dangerous in the event of a brain haemorrhage.
NB! Not for every patient it is suitable to administer thrombolysis.
The neurologist determines this immediately after a cerebral infarction has been diagnosed on the basis of various examinations. One of the most important conditions is that the stroke really occurred no longer than 4.5 hours.
In case of a ruptured cerebral blood vessel, an aneurysm, surgical intervention may sometimes help.
2. Stroke
(Hemorrhagic CVA)
This is a stroke caused by a blood vessel in the brain tearing or bursting. It is also called intracranial hemorrhage or intracerebral hemorrhage/hematoma, i.e. a hemorrhage in the cerebral blood vessels inside the skull.
Because part of the underlying brain tissue has no or insufficient blood supply and therefore receives insufficient or no nutrition and oxygen, this part may die.
Read more about specific topics:
Aneurysm, Dissection, SAH (subarachnoid hemorrhage/hematoma),
MMD, hereditary CAA /HCHWA-d, CAA, AVM, CCM, epidural hemorrhage (epidural hematoma), subdural hematoma, sinus thrombosis, intraventricular hematoma (IVH) in the ventricles/cerebral cavities and DADA2/ADA2 deficiency.

3. Cerebral infarction
(Ischemic CVA)
A cerebral infarction is caused by an interruption of blood flow through a cerebral artery (intracranial artery).
This leads to a lack of oxygen in the area that should supply that blood vessel with oxygen.
If such a sudden interruption of the supply of sufficient blood to the parts of the brain occurs, brain cells may die.
In the case of a cerebral infarction, for example, a blood vessel is blocked by a blood clot, or a blood vessel is seriously narrowed. As a result, part of the brain receives too little or no oxygen and that part can die.
A blockage of a blood vessel may be the cause, or a blood clot due to heart rhythm disorders or defects in the heart valve that allow clots to form.
There are more causes of a cerebral infarction: APS, Pica infarction (Wallenberg syndrome), CADASIL and RVCL, cortical infarction, subcortical infarction (without damage in the cortex or cerebral cortex), lacunar infarction (usually not caused by a clot but by vessel wall problems, for example due to high blood pressure, which causes a blockage due to the thickened vessel wall) and watershed infarction due to excessive drop in blood pressure.
Unfortunately, the cause of the infarction is not always found.
4. TIA
A TIA is a mild stroke caused by a temporary blockage of a blood vessel. TIA is the abbreviation for Transient Ischemic attack.
The blockage causes a shortage of blood (oxygen and nutrition) in certain brain cells (ischemia). The effects of a TIA do not last longer than 24 hours. If the symptoms persist for a longer period of time, it must be investigated whether there was a cerebral infarction after all.
Read more.
RIND
RIND (Reversible Ischemic Neurological Deficit) is a gradation between a TIA and a stroke / CVA.
The term is out of use today. There are reports that the symptoms of a RIND disappear completely and that is takes longer than 24 hours. It has been proven that a RIND can indeed cause permanent damage.
5. Sinus thrombosis
There may be a blood clot or several blood clots in the draining cerebral vessels. It is also called Cerebral Venous Thrombosis
(CVT). Read more.
6. Vascular wall problems
- These problems are caused by cerebral vasculitis, an inflammation of the blood vessels in the brain.
- Due to a rupture of the inside of the blood vessel (dissection)
people may suffer brain damage. This usually concerns the internal carotid artery (internal carotid artery) or the vertebral artery (vertebral artery) and the basal cerebral artery (basilar artery).
The latter artery is responsible for 20% of the brain's blood supply and runs at the bottom of the brain, the base. If the inside of the blood vessel ruptures, a 'false' aneurysm (balloon in the vessel wall) can develop. The resulting balloon can compress the blood vessel and result in an infarction.
Risk factors for a vessel wall rupture: high blood pressure, smoking, hereditary disorders, respiratory infection of the upper respiratory tract, an accident to the neck area or (hereditary) connective tissue or kidney disorders. If such a vessel wall rupture occurs, it is an acute and life-threatening situation.
7. Differences between cerebral hemorrhage, cerebral infarction, TIA
Cerebral Infarction or TIA
Blockage in the cerebral blood vessel
Cerebral hemorrhage
Blood flows from the cerebral blood vessel
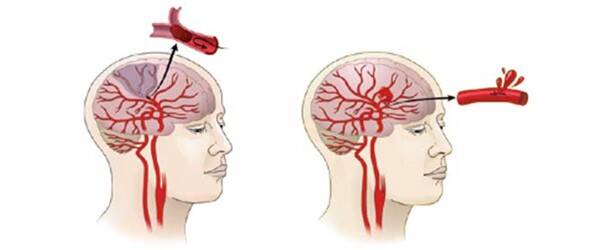
- Infarction: Oxygen and nutrition no longer pass through the blood vessel.
- TIA: The brain area temporarily does not receive oxygen and nutrition due to the temporarily closed blood vessel.
The underlying tissue is no longer supplied with blood (oxygen and nutrition) and will die. - Hemorrhage: Blood flows from the burst blood vessel pressing on brain cells.
You can watch videos about these kinds of brain injuries on YouTube:
8 . Injury on the right or on the left
Injury on the right
A stroke in the right hemisphere can leave the left side paralyzed
(and vice versa) or there will be a loss of strength.
This is caused by the fact that the nerve pathways cross from the right side of the head to the left side of the body (except in the case of damage to the cerebellum).
Paralysis or loss of muscle strength does not always occur.
Damage in the right hemisphere often results in other, less immediately noticeable disorders, which nevertheless hinder daily activities.
Injury on the left
If the left hemisphere is affected this often causes disorders in the use of language, both speaking and understanding.
The language and speech center is located in the left hemisphere of right-handed people. If there is loss of strength or paralysis, it is in the right side of the body because the nerve pathways cross from the left hemisphere of the brain to the right side of the body.
This is called contralateral, on the opposite side.
The crossing of nerve pathways to the body takes place in the medulla oblongata.
In case of injury to the cerebellum, loss occurs on the same side of the cerebellum as in the body.
This is called ipsilateral, on the same side. Injury to the right side of the cerebellum will cause problems in the right half of the body.
9 . Recognize a stroke quickly
The sooner you get to the hospital the better.
In some cases, powerful medications that dissolve the blood clot can resolve the blockage of the artery in the brain during a cerebral infarction, limiting the damage.
This should start within four and a half hours after the first symptoms of a stroke.
Women more often show atypical symptoms, such as disorientation, confusion and/or loss of consciousness.
In case doubt, be on the safe side and call the emergency telephone number!
Quick check:
Mouth, Speech, Arm = Stroke alarm
FAST = Face, Arm, Speech, Time (record the time)
Note the time of the stroke and call the emergency telephone number!
People in the hospital will want to know this, because the treatment of a stroke that has occurred recently is different from an older stroke.
All symptoms: (symptoms vary per person)
These are the alarm bells:
Some complaints are isolated and are the only complaint mentioned.
- Sudden weakness or paralysis in the arm, leg, or on one side of the body; in arm or leg. Sleeping leg. Not being able to steer your arm properly, as if your arm has a life of its own. Not able to write anymore
- Numbness on one side of the body
- Drooping half of face; one corner of the mouth, one eyelid
- The pupil of that eye with drooping eyelid may be very small
- Decreased vision with one or both eyes
- Loss of vision, shrinking field of vision. Dark spot in the corner of the eye
- Sudden loss of vision in one eye, drooping eye or double vision. Rolling eyes
- Decrease in power
- Decrease in coordination
- Dizziness Vertigo, often accompanied by nausea, vomiting, fever, hiccups or difficulty swallowing. Balance disorders
- Very bad headache. Stabbing headache. Migraine. The sudden onset of a very severe headache. Sometimes there is a feeling as if pins are stuck in the head.
- Decreased consciousness, loss of consciousness or sudden drowsiness
- Slurred speech, Language problems, speaking more slowly or with difficulty
- Difficulty understanding spoken language
- Disorientation, confusion, not quite being in the here and now
- Nausea and vomiting
- Difficulty swallowing or coughing
- Just toppling over
- Some behave as if they are drunk
- Emotional lability
- Difficulty breathing
It has happened that people have been sent home with a burnout diagnosis. Later it turned out to be a stroke.
Recognize a stroke!
wasting time is wasting a brain
Call the emergency telephone number!
11. Consequences of a stroke / CVA
Physical consequences
A half-sided paralysis (right or left sided hemiplegia) or weakness (hemiparesis) in the arms, hands, face, chest, legs or feet can lead to all kinds of problems.
Muscle weakness is often characteristic in the initial phase. Later, it is more likely to be disturbances in coordination and spontaneous, often annoying contraction of muscles (spasms) or spasticity.
On the physical consequences page we discuss in detail all possible physical consequences.
Emotionally and behaviorally
Consequences ranging from depression to uninhibited emotions occur.
For all consequences, see the consequences on emotion and behavior page.
Cognitive
- Slow thinking
- Memory weakness
- Aphasia - problems with language
- Apraxia - difficulty with multiple actions
- Neglect - neglecting the left or right side of the body
- Agnosia – no longer recognizing people or objects
The list is so long that we have a specific page about it:
invisible consequences of brain injury
People who have had a stroke experience many limitations. People who are recovering may also have difficulty moving again.
13. Stroke risc factors
- Age; From the age of 55, the risk of developing a cerebral infarction doubles with every ten years that pass.
- Sex; Stroke is more common in men than in women.
- Family history
- Own history. Someone who previously had cardiovascular disease has a greater risk.
- High bloodpressure. A blood pressure higher than 130/80 is a risk. Discuss this with your GP or during the CVR consultation hour. (CVR: Cardiovascular Risk Management)
- Diabetes
- Smoking and alcohol consumption
- Atrial fibrillation is a common heart rhythm disorder with palpitations, irregular heartbeat, usually fast heartbeat, shortness of breath, fatigue, dizziness, fainting, chest pain, reduced ability to exercise, or asymptomatic (not showing any symptoms). There can be one blood clot in the heart atrium. Such a blood clot can break loose and block a blood vessel somewhere else in the body, such as in the brain.
- Contraceptive pill use; Not specific for a cerebral hemorrhage, but for the development of clots in the blood. As a result, there is a chance of having a cerebral infarction. This applies in particular to "the third generation pill" in combination with overweight BMI over 30), pregnancy (with especially the last three months or around the time of delivery).
- Blood clotting disorders.
- High cholesterol levels in the blood. Blood values above 200 mg/dL indicate a risk of arteriosclerosis.
- Overweight. Therefore, try to keep the weight at the right level. Adapt the food you eat and the foods you consume to your body.
- Certain stress-increasing character traits.
- Little exercise. Try to exercise at least half an hour a day. Every little exercise helps.
- Eating too little fruit and vegetables. Therefore, eat at least 200 grams of vegetables (= 250 grams of prepared vegetables) and 2 pieces of fruit every day and be careful with salt.
- Since 2020, a specific type of stroke (sinus thrombosis) has been linked to vaccination against the coronavirus as a possible side effect. (COVID-19)
Specific risk factors for cerebral haemorrhage
In addition to the risk factors already listed, there are various abnormalities and factors that can increase the risk of a cerebral hemorrhage.
- Vascular abnormalities. In the 2nd to 3rd week of pregnancy, something can go wrong in the development of the blood vessels. For example, an arteriovenous malformation (AVM). This is usually not hereditary.
- Aneurysm in the brain. If a dilation, a kind of bulge, occurs in the wall of the artery, it may grow and suddenly burst open. This causes bleeding. This hemorrhage often occurs in the space between the skull and the brain in the subarachnoid space (subarachnoid hemorrhage or SAH).
- a congenital weak spot in the vessel wall
- high bloodpressure
- smoking and excessive alcohol consumption
- bacterial infection of the vessel wall (very rare)
- improperly formed blood vessels
- a congenital weak spot in the vessel wall
- Clotting disorders. This does not cause bleeding, but it can increase the consequences of a cerebral hemorrhage. See also our page
rare blood diseases. - Cerebral Amyloid Angiopathy (CAA) Special protein accumulations (amyloid) can cause blood vessels to become less flexible and damaged. Bleeding like consequences of CAA mainly occur in the elderly. A hereditary form of CAA is HCHWA-d or Katwijk disease.
- Use of anticoagulant medications
Reduce risk
Food and drink:
- eat healthy and varied food. Eat lots of vegetables and fruit.
- use as little salt as possible.
- watch your fat consumption. Use little fat. Unsaturated fats are healthier than saturated fats.
- alcohol consumption maximum one normal glass per day.
Exercize:
- Sufficient exercise, at least half an hour a day
- Weight: try to maintain a healthy weight
- Smoking and drugs: try to avoid it.
14. Rare blood diseases
There are various blood diseases or bone marrow diseases in which the blood does not clot sufficiently or clots too much or in which too little blood is produced. In the first case, this can lead to bleeding such as cerebral hemorrhage and in the second case, clotting too quickly can lead to cerebral infarctions. If too little blood is produced, this can also cause brain damage in the long term. Read more on our special page about rare blood diseases.
15. Stress and high blood pressure as causes and genetic cuases
Persistent stress is a cause of stroke (CVA), studies in eastern Finland showed. 113 strokes (90 cerebral infarctions) occurred in 11.2 years of follow-up in 2303 men. Men with elevated systolic blood pressure (>/= 20 mm Hg) had a 72% greater risk of stroke and 87% greater risk of cerebral infarction compared to men who were less responsive to stress.
Moreover, people with a low level of education were almost 3 times more likely to have a stroke than those with better education.
Read more. High blood pressure increases the risk of a heart attack, stroke or heart failure. This makes high blood pressure/hypertension one of the leading causes of death or permanent injury worldwide.
A research team, led by scientists from Maastricht University (UM), suspects that high blood pressure is the result of a certain protein (Nox5) that is the source of so-called oxygen radicals in the walls of blood vessels. These radicals disrupt a process that normally helps to prevent narrowing of the arteries and thrombosis formation. This could be solved within a few years with simple medicines.
16. Genetic Causes
There are several forms of a cerebral infarction or cerebral hemorrhage that have a hereditary component.
- ADA2 deficiency (DADA2)
- Antiphospholipid syndrome APS
- CADASIL (Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy)
- CARASIL (cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy)
- Cerebrotendinous xanthomatosis (CTX)
- Ehlers-Danlos syndrome (vascular EDS)
- Hereditary CAA (HCHWA-D)
- Factor V Leiden
- Fibromuscular dysplasia
- Homocystinuria
- MELAS (Mitochondrial encephalomyopathy, lactic acidosis and stroke-like episodes)
- Moyamoya syndrome
- Reus cell arteritis (temporal arteritis or arteritis temporalis)
- Sickle cell disease (SCD) Sickle cell anemia
- Marfan syndrome
- Rendu-Osler-Weber syndrome (Rendu-Osler-Weber syndrome, ROW, telangiectasia familiaris haemorrhagica, hereditary hemorrhagic telangiectasia) Type 1 has more problems with the lungs and brain than type 2.
- Sneddon's syndrome
- Susac's syndrome
- Vasculitis
- Vasculopathy associated with ADA2 mutations
- Fabry disease
People with a family history of stroke are also likely to share potential contributing factors.
17. Silent cerebral infarction SCI (unnoticed cerebral infarction or silent cerebral infarctions)
About 20% of apparently healthy people over the age of sixty have ever had a 'silent', unnoticed cerebral infarction. Such a silent, unnoticed cerebral infarction is called an SCI. SCI stands for silent cerebral infarctions.
It can leave small scars in the brain that are discovered accidentally during a brain scan. These small scars are most often seen in the basal ganglia (52%), other subcortical areas (brain areas located under the cerebral cortex) (35%) and cortical areas (brain areas within the cerebral cortex) (11%).
Such a silent infarction can be a warning of an increased risk of a cerebral hemorrhage or cerebral infarction (stroke) and dementia.
Read more about research into SCI.
18. Young stroke
Although strokes are often associated with the elderly, they can also occur at a younger age! Unfortunately, this is not always recognized.
Causes can vary from hereditary factors, blood vessel abnormalities and heart problems to lifestyle-related causes.
People who have suffered a cerebral haemorrhage, cerebral infarction or an abnormality of the cerebral vessels at a young age (under 50) belong to the group of people with 'young stroke'. That is to say: young people with a stroke.
They often have different needs and rehabilitation requirements than the elderly. For example, help with work, family, school, study, relaxation and sports. Ask about Young stroke rehabilitation.
For more information:
- Young stroke Foundation Australia
- Young Stroke Survivors UK
- BMC Public Health
- Medical Research Foundation